-
PDF
- Split View
-
Views
-
Cite
Cite
Kit-fai Lee, Randolph H L Wong, Howard H W Leung, Eugene Y J Lo, Charing C N Chong, Anthony W H Chan, Paul B S Lai, En bloc transdiaphragmatic lung resection for locally advanced hepatocellular carcinoma: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa084, https://doi.org/10.1093/jscr/rjaa084
Close - Share Icon Share
Abstract
A 56-year-old man presented with an 11-cm hepatocellular carcinoma (HCC) at segment 7 of liver. To induce left liver hypertrophy, a sequential transarterial chemoembolization (TACE) and portal vein embolization before right hepatectomy were adopted. However, the tumor further increased in size despite TACE and invaded through the diaphragm to the right lung base. Anterior approach right hepatectomy with en bloc wedge resection of the involved right lower lobe of lung by endovascular staplers via transdiaphragmatic approach was performed. The diaphragmatic defect was closed with Goretex mesh. Patient made an uneventful recovery. Pathology confirmed a 12.5 cm poorly differentiated HCC invading through diaphragm to lung. During follow-up, patient developed a 6 cm recurrence at left lung base 17 months after surgery for which he received sorafenib therapy. However, the lung mass further increased in size with new liver recurrence at segment 3 despite treatment. He succumbed 2 years and 3 months after surgery.
INTRODUCTION
Due to its close relation, hepatocellular carcinoma (HCC) with invasion of diaphragm is not a rare occurrence [1]. However, direct invasion of HCC to lung base through diaphragm is rare [2]. Here, we would like to report a case of en bloc resection of involved lung base via a transdiaphragmatic approach during right hepatectomy for a large HCC.
CASE REPORT
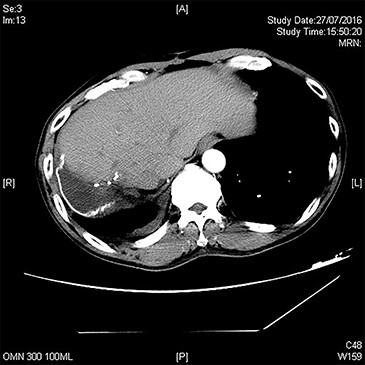
A 56-year-old man who enjoyed good past health presented with right upper quadrant abdominal pain and fever for 2 weeks. Blood tests revealed normal complete blood counts, liver and renal function. Computed tomography (CT) of abdomen revealed an 11 cm mass at segment 7 of liver compatible with HCC. Patient was found to be a hepatitis C carrier and his serum alfa-fetoprotein (AFP) was elevated to 355 μg/l. Right hepatectomy was planned but due to small left liver size and borderline indocyanine green liver function test, patient was offered sequential transarterial chemoembolization (TACE) and portal vein embolization (PVE) before surgery [3].
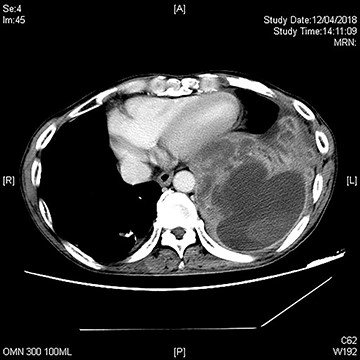
A repeat CT after TACE and PVE though showed sufficient hypertrophy of left liver, it also revealed significant growth of tumor with invasion to right lower lobe of lung through diaphragm (Fig. 1). Operation proceeded with a Mercedes-Benz incision with patient placed in supine position. Tumor was found to invade through medial part of diaphragm to right lower lobe of lung for 3 cm depth. Anterior approach right hepatectomy was performed [4]. Diaphragm was divided surrounding the tumor invasion site. En bloc wedge resection of the involved right lower lobe of lung was performed with endovascular staplers via the diaphragmatic opening. The diaphragmatic defect was closed with Goretex mesh (Fig. 2). Patient made an uneventful recovery and went home on Day 8 after surgery. Pathology confirmed a 12.5 cm poorly differentiated HCC invading through diaphragm to lung (Figs 3 and 4). Both resection margins at liver and lung were >1 cm. AFP decreased to 3 μg/l after operation.

CT showing a large hepatocellular carcinoma invading through diaphragm into lung base. (A) axial view, (B) coronal view and (C) sagittal view. Hyperdense material within liver is lipiodol deposits after previous TACE.
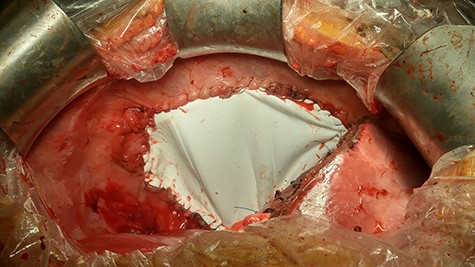
Operative view showing the diaphragmatic defect closed with Goretex mesh.
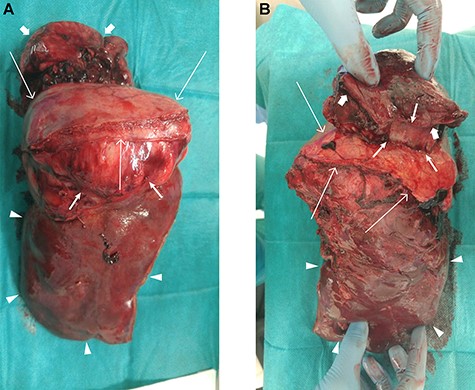
Resected specimen showing right lobe of liver (arrow heads), diaphragm (long arrows), tumor (median arrows) and resected lung tissue (short arrows). (A) Lateral view and (B) medial view.
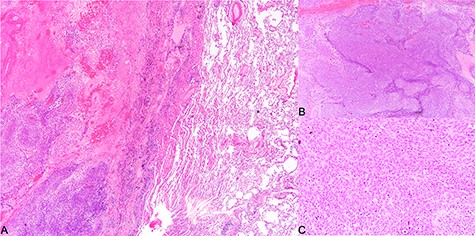
Histological findings. (A) Tumor invading into lung parenchyma, (B) tumor arranged in solid sheets (×40) and (C) tumor cells of the poorly differentiated hepatocellular carcinoma (×200).
Follow-up CT showing hypertrophied left liver without recurrence.
Serial CT after surgery did not reveal recurrence (Fig. 5) until 17 months post-operation when patient developed hemoptysis. CT thorax revealed a 6-cm soft-tissue mass at left lower lobe of lung (Fig. 6). Bronchoscopy revealed a necrotic endobronchial growth at left lower bronchus orifice. Biopsy finding of tumor growth was compatible with HCC. Patient was given sorafenib for recurrent HCC at left lung. Repeat CT 5 months later revealed further increase in size of lung mass and a new segment 3 liver lesion suggestive of liver recurrence. AFP remained at around 3 μg/l even in late stage of recurrent disease. Patient’s general condition continued to deteriorate and succumbed 2 years and 3 months after surgery.
DISCUSSION
Liver resection remains an important curative treatment for HCC. When future liver remnant is considered inadequate, PVE is a commonly employed technique to induce liver hypertrophy. It usually takes 4–6 weeks for sufficient liver hypertrophy to take place. One round of TACE was commonly performed 4 weeks before PVE to suppress tumor growth during this waiting period. Such sequential TACE and PVE strategies were applied in our patient [3]. However, the tumor progressed despite TACE and even invaded the lung base through the diaphragm.
When diaphragm is invaded by tumor, en bloc resection is advised if this is the only obstacle for oncological clearance [1]. Direct invasion of lung base through diaphragm is a rare occurrence. Only one report of en bloc resection of liver, lung and diaphragm for HCC was found in literature [2]. That patient was alive without recurrence 10 months after surgery. In our case, thoracotomy was avoided as the limited lung resection could be performed through the diaphragmatic defect after diaphragmatic resection. This could have decreased postoperative chest complication and hastened patient recovery. Otherwise, patient would need a thoracoabdominal incision for adequate exposure for diaphragmatic and lung resection. Similar technique has been described for simultaneous lung and liver resection for synchronous liver and lung metastases and was shown to reduce blood loss and hospital stay as compared with staged hepatectomy and thoracotomy [5].
Our patient developed recurrence at contralateral lung base 17 months after operation. It was more compatible with endobronchial metastasis as tumor was visualized by bronchoscopy [6]. According to Kiryu et al. [7], endobronchial metastasis consists of the following types: type I, direct metastasis to the bronchus; type II, bronchial invasion by a parenchymal lesion; type III, bronchial invasion by mediastinal or hilar lymph node metastasis and type IV, peripheral lesions extended along the proximal bronchus. Our patient probably belonged to type I or type II metastasis.
Another unusual finding was the normal AFP value despite recurrent disease. This might have represented a new cell line of tumor, which was different from the primary tumor. A serum AFP level above 400 μg/l has been shown to predict poor overall and recurrence-free survival after hepatectomy in patients with HBV-associated HCC [8]. Our patient also got high AFP (almost reached 400 μg/l) before operation.
Our patient survived 2 years and 3 months after surgery. Given the initial large poorly differentiated tumor with involvement of lung and diaphragm, such survival was reasonable. It should be noted that the patient did not suffer from recurrence at resection site implying a good local control of disease was obtained with radical surgery.
In summary, transdiaphragmatic en bloc lung resection is feasible and safe in selected cases of HCC with invasion to diaphragm and lung base, allowing oncological clearance and reasonable survival.
Funding
This study was not supported by any grant or funding.
Conflict of interest statement
None declared.
References
- lung
- carcinoma, hepatocellular
- follow-up
- hepatic resection
- surgical mesh
- surgical procedures, operative
- respiratory diaphragm
- hypertrophy
- liver
- neoplasms
- pathology
- surgery specialty
- lung volume reduction
- wedge resection
- portal vein embolization
- advanced adult primary liver cancer
- sorafenib
- lung mass
- right lung
- defect of diaphragm
- left lung
- lobe of lung
- transarterial chemoembolization
- lung excision



