-
PDF
- Split View
-
Views
-
Cite
Cite
Nabila Salhab, Bardisan Gawrieh, Mohammad Ali Deeb, Norma Taishori, Ammar Omran, Classic bladder exstrophy and complete rectal prolapse in a 10 year-old child with no previous surgical intervention: what to achieve?, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa093, https://doi.org/10.1093/jscr/rjaa093
Close - Share Icon Share
Abstract
The management of bladder exstrophy (BE) remains one of the most significant challenges encountered by pediatric urologists despite improvements in the operative techniques worldwide. Regardless of surgical technique, timing of primary closure remains a matter of debate. The initial closure may be performed within the first 48–72 hours of life or at ~6–12 weeks of age. Delayed presentation until adolescence is extremely rare. However, due to lack of awareness, and access to healthcare along with poor socioeconomic conditions in developing countries, some patients may not receive treatment during infancy. We present a case of a 10-year-old Syrian male with BE associated with complete rectal prolapse who did not undergo any previous surgical interventions.
INTRODUCTION
Bladder exstrophy (BE) is a rare congenital anomaly that occurs with a reported prevalence of 3.5 per 100 000. In classic BE, the bladder is completely opened in the lower abdomen so the edge of inner surface is fused to the abdominal skin combined with epispadias [1, 2]. Common problems in subsequent years include issues related to continence, sexual function and the appearance of lower abdomen and genitals. However, when addressed during infancy, satisfactory results could be achieved [3].
CASE PRESENTATION
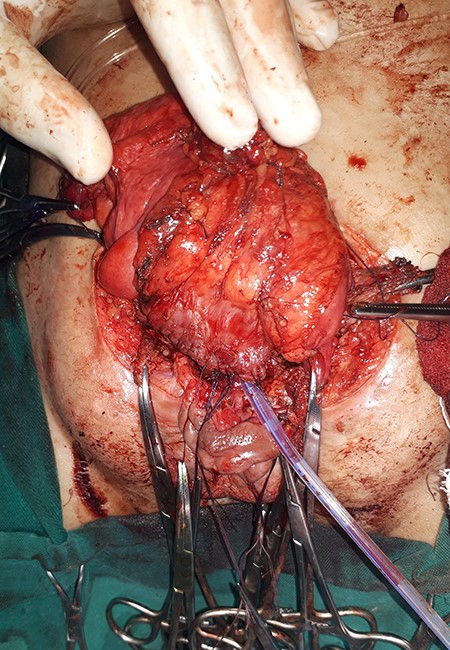
A 10-year-old Syrian male presented to our department with bladder exstrophy, having not undergone any surgical intervention prior due to social and financial reasons. Physical examination revealed classic bladder exstrophy and multiple large polyps on the mucosal surface. Complete rectal prolapse (Fig. 1) due to a significant widening of the pubic symphysis and the levator ani complex were also divergent, leading to weakness in the pelvic floor as well as fecal incontinence. After admission, the child undergone full blood and urinary tests and intravenous pyelogram, and the results of all were normal. Ultrasound of the urinary tract was performed, and no associated anomaly of the upper urinary tract was detected. The decision was to perform complete bladder closure with augmentation and preservation of the bladder template for reimplanting the ureters and using the dilated sigmoid for augmentation. As a first step of reconstructing this complicated anomaly, bilateral anterior oblique iliac osteotomies via separate incisions were performed. Traction sutures were placed into the glans penis, and ureteral catheters were secured in each ureteral orifice. An incision was made around the periphery of the exstrophic bladder plate, and a plane of dissection was established between the rectus fascia and bladder. Dissection was continued toward the pubis, and the incision was then extended distally to the verumontanum on both sides of the prostatic urethra, leaving a wide strip of bladder neck and urethral plate. Reimplanting the ureters on the bladder template was done using modified Lich–Gregoir reimplantation. The next step was the augmentation of the bladder (Fig. 2) using the dilated sigmoid. After isolating a segment of sigmoid about 10 cm, we opened the segment along its anti-mesenteric border and then sutured it to the opened bladder template. A cystostomy tube was performed depending on Monti’s procedure by using a part of the augmented bladder (Fig. 3). We used a 16 Fr catheter, and the stoma was made at the level of the new umbilicus. End-to-end anastomosis was performed on the divided sigmoid, and the rectum was ligated to the sacrum with 2\0 Prolene sutures. Ureteral catheters were removed 14 days after surgery. At 3-month follow-up, upper urinary tract imaging studies and urine tests were normal, and the patient did not suffer from any anorectal problems. The patient is prepared for bladder neck reconstruction and epispadias repair. As soon as bladder neck reconstruction is performed, the child will be ready for continence training (Fig. 4).

Classic bladder exstrophy and complete rectal prolapse in a 10-year-old male.
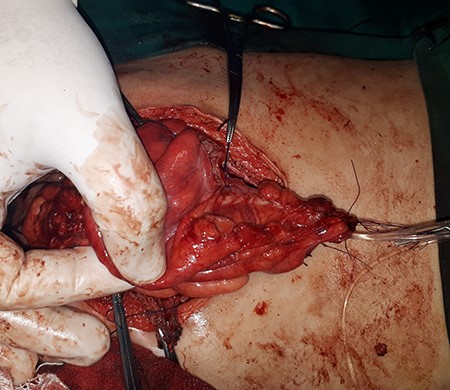
A cystostomy tube depending on Monti’s procedure by using a part of the augmented bladder.

DISCUSSION
The current primary objectives of surgical management of classic bladder exstrophy are to close the abdomen and bladder, establish urinary continence with the preservation of renal function and provide acceptable external genitalia [3, 4]. This is best initiated in the neonatal period, where results of primary reconstruction appear satisfactory [4, 5]. The unique aspect of this case was the age of the child, keeping in mind the challenges that come with delaying intervention, including a very small bladder plate, polyps all over its surface associated with complete rectal prolapse. There seems to be little experience in dealing with bladder exstrophy at this age, as relevant cases reported in medical literature are quite few. The main concern in our case was to close the abdomen and bladder and to deal with the rectal prolapse issue, which could have an unfavorable effect on the child’s social life and schooling. We preserved the bladder template because of its significant advantages, as Gearhart suggested that the preservation of the bladder comes with many benefits, such taking less bowel for augmentation. Furthermore, if urethral reimplantation was necessary, as in our case, the bladder template was a much better place for reimplantation than a bowel wall [6]. Preserving the bladder plate is not without controversy, especially when exposed to the environment for a long time, as is the case with subject of this report, and the potential of malignancy involved. However, Engel concluded that histological changes were present in all bladders, including those of neonates, and that malignant transformation was not prevented by closure of the exposed bladder plate even during the neonatal period [7]. Ureterosigmoidostomy was the established form of urinary diversion for patients with bladder exstrophy when bladder reconstruction is not possible or has failed. Made it possible for patients to have a good body image and social integration because they do not have to wear a bag and there is no stoma on the anterior abdominal wall [8]. Ureterosigmoidostomy still has long-term problems, including ascension of bacteria to the upper urinary tract, hypokalemic acidosis, rectal incontinence, ureteral obstruction and delayed development of malignancy [9]. Thus, we chose to perform bladder augmentation with continent urinary diversion using the dilated sigmoid and fixing the rectal prolapse at once, as the child was at a proper age for clean, intermittent catheterization. The child presently visit our department for follow-up urine tests and ultrasonography, and he is progressing well and is prepared for the next stages of epispadias repair and bladder neck reconstruction 6 months following the first operation.
In conclusion, we described a case of a 10-year-old Syrian male with BE associated with complete rectal prolapse who admitted to our low volume center and had bladder augmentation and rectum fixation, and the results were acceptable so far in a short-term follow-up.



