-
PDF
- Split View
-
Views
-
Cite
Cite
Cláudia Leite, Débora Aveiro, Rosa Simão, Sandra Coelho, Carlos Casimiro, Laparoscopic repair of Morgagni’s hernia in an elderly female patient, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa182, https://doi.org/10.1093/jscr/rjaa182
Close - Share Icon Share
Abstract
Morgagni’s hernia is a very uncommon congenital diaphragmatic hernia. A few patients may remain asymptomatic until adulthood. Clinical presentation may include bowel obstruction, chest pain or dyspnoea. The authors report the case of a 71-year-old female patient, admitted to the emergency department due to respiratory symptoms, whose thoracic computed tomography revealed a large Morgagni’s hernia, containing colon. She underwent an elective laparoscopic repair with mesh. Thoracic computed tomography is the best imaging study for its diagnosis. Laparoscopic repair is safe and allows symptomatic relief and incarceration risk reduction.
INTRODUCTION
In 1761, Morgagni described the classical anterior diaphragmatic hernia. It accounts for only 5–10% of congenital diaphragmatic hernias (CDH) [1]. The estimated prevalence of CDH is 1/2000 to 1/5000 live births [2]. In total, 61% of cases occur in females [3]. The ‘foramen’ of Morgagni’s hernia occurs in the anterior midline of the diaphragm, predominantly on the right side.
A few patients may remain asymptomatic until adulthood [4]. Clinical presentation may include obstructive symptoms from protrusion of the colon, epigastric or chest pain and dyspnoea, to name just a few.
The finding of mediastinal abnormalities on a chest X-ray, such as widening or air-fluid levels, should raise suspicion of a diaphragmatic hernia. Thoracic computed tomography (CT) is the gold-standard imaging study for determination of its content and ‘foramen’ localization.
Surgical repair is recommended for all fit patients [5], preferably through a minimally invasive approach.
CASE REPORT
The authors report the case of a 71-year-old female patient, back to the year of 2018, with a past history of mild asthma, otherwise healthy, who was admitted to the emergency department due to an upper respiratory tract infection. Upon examination, there seemed to be bowel sounds on the thorax, heart sounds were slightly diminished and the abdomen was flat.
She had a chest X-ray done (Fig. 1) that showed widening of the mediastinum, as well as a few air-fluid levels, which raised suspicion of a diaphragmatic hernia. She also had a thoracic CT done (Fig. 2) that revealed a large hernia in the anterior mediastinum, containing transverse colon and a significant amount of ‘omentum,’ causing right side heart deviation.

Chest X-ray showing widening of the mediastinum and a few air-fluid levels
She had neither history of fall from height nor car crash, but described episodes of epigastric pain, particularly on bending forward.
Subsequently, she was referred to General Surgery and offered elective surgical repair of the hernia. Then, she underwent a laparoscopic repair, through 4 trocars (2 of 10 mm
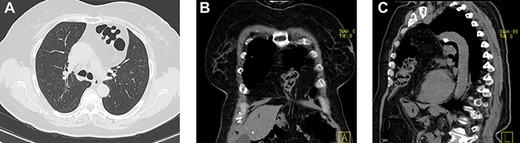
(a–c) Axial, coronal and sagittal images, respectively, of thoracic and abdominal CT showing the localization of this hernia.
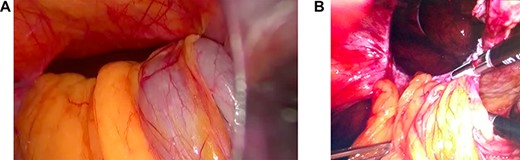
(a and b) Photographs taken during surgery: herniated colon and ‘omentum,’ and after reduction of these contents, respectively.
on the umbilicus and left hypochondrium, and another 2 of 5 mm on the right hypochondrium and left flank), with gentle reduction of all herniated content (transverse colon and greater ‘omentum’) (Fig. 3), adhesiolysis, measurement of the defect (5 cm in diameter) and placement of a dual face mesh, consisting of polytetrafluoroethylene (PTFE) and polypropylene, from ‘Bard Dulex’®, of 8 × 12cm (Fig. 4), that was fixed with absorbable tackers from ‘Ethicon’® and a few anchoring sutures of a monofilament non-absorbable thread (polypropylene). The procedure ran uneventfully.

Photograph taken during surgery: placement and fixation of the mesh.
She had a chest X-ray done on the first postoperative day that showed no thoracic complications (pneumothorax nor hemothorax). She had an uneventful recovery and was discharged home on the third postoperative day.
Follow-up at the first and fourth postoperative months, remaining clinically asymptomatic. At the fourth postoperative month, she had a follow-up thoracic and abdominal CT done (Fig. 5) that confirmed no mesh migration nor hernia recurrence.
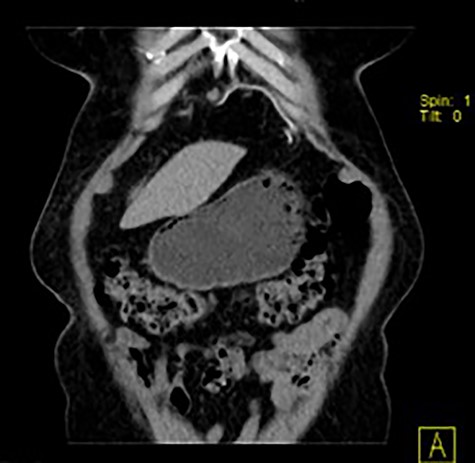
Coronal image of thoracic and abdominal CT showing the location of the mesh (linear and hyperdense).
DISCUSSION
Once a patient presents a widening of the mediastinum, shifting of heart and mediastinum (usually to the right), or presence of thoracic air-fluid levels on a chest X-ray, one should always consider the possibility of a diaphragmatic hernia, regardless of their age.
Generally speaking, the lesser the diaphragmatic defect the later will the patient become symptomatic. Twenty-eight percent of patients are asymptomatic at the time of diagnosis [3]. Our patient remained nearly asymptomatic until elder hood. The aging process is naturally associated with muscular weakening and thinning, accompanied by visceral fat and intra-abdominal pressure increases.
Clinical presentation may vary from subtle and insidious respiratory or functional digestive symptoms, to life-threatening conditions, such as bowel obstruction or ischemia, gastric or splenic volvulus and significant pulmonary dysfunction. Our patient had a past history of mild asthma, therefore she may not have realized the decline in her pulmonary compliance and exercise tolerance.
The risk of an emergency presentation is between 12 and 14% [6]. This is the rationale that supports the recommendation of an elective surgical repair for all fit patients, even if asymptomatic [7]. Our patient received respiratory kinesiotherapy prior to surgery, as it is proved to improve outcomes.
Laparoscopic repair is an attractive approach, as it has recurrence and complication rates that are similar to open repairs. The recurrence rate is very low (2.3%) [8]. Our patient had transverse colon and a large amount of greater ‘omentum’ herniated toward the anterior mediastinum, which required gentle traction with atraumatic graspers. According to a recent review, hernia contents include large bowel (in 72% of cases), ‘omentum’ (65%), small bowel (25%), stomach (4%) and fat (2%) [8].
Mesh placement is recommended for defects larger than 3 cm [9], as was the case in our patient. We chose a dual face mesh: polypropylene and PTFE for the thoracic and abdominal sides, respectively, since PTFE is deemed to be less prone to adhesions and fistulae formation [10]. Ideally, there should be a 2 cm overlap between the mesh and the border of the defect, so as to preclude recurrence, because meshes may shrink over time.
Thoracic CT is the gold-standard imaging study for determination of the content and localization of the ‘foramen’ of its hernia. Currently, urgent thoracic CT has been more frequently requested, so as to clarify some respiratory conditions, which has allowed us to detect asymptomatic diaphragmatic hernias, and properly refer these patients to surgery. It has been estimated that the diameter of the defect may grow up to 7 mm per year, if left untreated [8].
To conclude, in the absence of a past traumatic history, the radiographic finding of widening of the mediastinum with air-fluid levels, and a relative paucity of air below the diaphragm, should raise suspicion of a congenital diaphragmatic hernia, regardless of patient age. Even in asymptomatic patients, the defect enlarges and stretches with aging, and life-threatening complications may arise. Thus, an elective surgical repair should be offered to all fit patients.



