-
PDF
- Split View
-
Views
-
Cite
Cite
Emanuel Mejias, Yarret Robles, Gerardo Olivella, Guillermo Bolaños, Gouverneur’ syndrome in a young Hispanic patient: A case report of a rare presentation of a rectal adenocarcinoma tumor, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa064, https://doi.org/10.1093/jscr/rjaa064
Close - Share Icon Share
Abstract
This is an unusual case report of 32-year-old Hispanic male who presented with an early-onset advanced stage colorectal cancer with an enterovesical fistula. A 32-year-old man presented to our institution referring suprapubic pain, urinary frequency, dysuria and tenesmus for several weeks suggesting Gouverneur’s syndrome. Patient had been treated with oral antibiotics for his recurrent urinary tract infections without resolution. Associated unintentional weight loss, decreased appetite and suprapubic pain raised concern for occult malignancy. Abdominopelvic computed tomography scan revealed a rectal mass with invasion to bladder. Colonoscopy biopsy confirmed diagnosis of moderately differentiated rectal adenocarcinoma. This report provides vital information about clinical presentations of enterovesical fistula in an imposed rectal adenocarcinoma in a young Hispanic adult with no previous family or medical history. A thorough clinical assessment must be taken to ensure accurate diagnosis and early detection of colorectal cancer in the young Hispanic population.
INTRODUCTION
Clinical evaluation of suprapubic pain, frequency, dysuria and tenesmus have been described as the hallmark presentation of enterovesical fistula (EVF), also known as Gouverneur’s syndrome [1]. EVF may present secondary to inflammatory disease, tumors or traumatic injuries, producing abnormal communication between the intestine and the bladder [1, 2]. Rectal adenocarcinoma, an epithelial growth tumor, has been associated with long standing EVF in patients with inflammatory disease in multiple studies [3, 4]. However, to our knowledge there are no previously reported cases of Gouverneur’s syndrome in young Hispanic adult patients secondary to rectal adenocarcinoma. The purpose of this article is to describe a case of a young Hispanic adult patient with pneumaturia and recurrent urinary tract infections caused by an EVF secondary to rectal adenocarcinoma.
CASE REPORT
A 32-year-old man with no past medical or surgical history presented to the emergency department (ED) in April 2018, distressed and complaining of worsening pneumaturia for the past 3 days. The patient reported a 2-week history of polyuria, dysuria, suprapubic pain, tenesmus and inability to control his sphincters, prior to the ED-onset presentation. Further history revealed a 50-pound involuntary weight loss in a 5-month period, with partially treated urinary tract infections without resolution. He denied toxic habits, high-risk sexual behavior nor family history for colorectal cancer or inflammatory bowel disease. Based on the symptoms described, the rare triad of Gouverneur’s syndrome related to the EVF was considered. Physical evaluation revealed no palpable anorectal masses, adequate rectal tone and no visible gross blood. Urine analysis showed pyuria, hematuria, proteinuria with urine culture positive for Escherichia coli. Abdominopelvic computed tomography (CT) scan showed circumferential wall thickening of the rectum with surrounding fat stranding and numerous prominent pelvic lymph nodes (Fig. 1). Additionally, the scan showed pericolonic gas and fluid collection with a fistulous tract adjacent to the proximal rectum and the bladder (Fig. 2). In Figure 3, two hepatic hypodense lesions located in the right lobe of the liver were identified suggestive of metastasis. During colonoscopy, at approximately 20 cm from the anal verge a large, firm, irregular, friable, concentric mass was identified obstructing 95% of the lumen (Fig. 4). During surgery, the mass was not amenable for resection, due to its low pelvic location and size; a loop colostomy was performed for decompression, with liver tru-cut needle biopsy. Intraoperative cystoscopy was unsuccessful in placement of ureteral stents due to tumor invasion to the bladder.
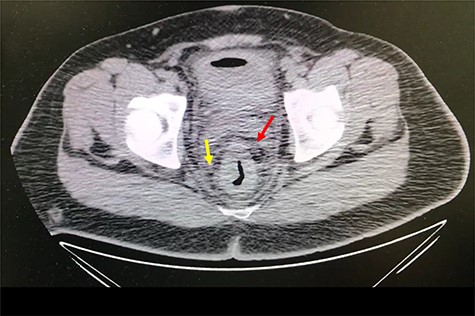
Axial abdomen and pelvis CT scan showing enlarged lymph nodes (yellow arrow) and fat standing around rectum (red arrow).
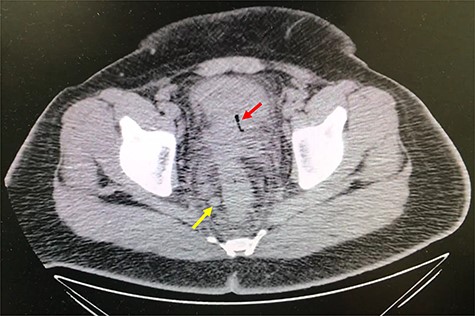
Axial abdomen and pelvis CT scan showing fistulous tract adjacent to the proximal rectum and the bladder (red arrow) and enlarged lymph nodes (yellow arrow).
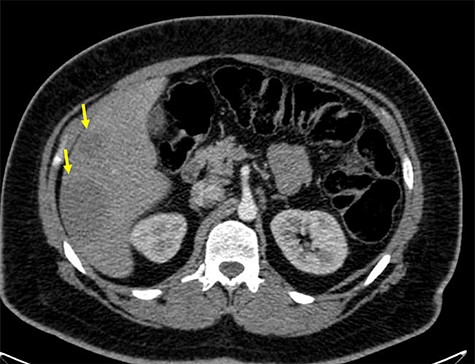
Axial abdomen and pelvis CT scan showing hepatic hypodense lesion and possible liver metastasis (yellow arrow).

Colonoscopy results showing a large, irregular, friable concentric lesion occluding 95% of the lumen, 20 cm from the anal verge.
Pathology report from mass biopsy revealed a moderately differentiated rectal adenocarcinoma, with carcinoembryonic antigen (CEA) (+) and alpha fetoprotein (AFP) (+) levels.
DISCUSSION
Multiple studies have shown an increasing trend in colorectal cancer (CRC) diagnosis in the younger population [5–7]. In 2015, Bailey et al. reported a growing incidence rate (10%) among patients from 20 to 50 years with a 20% reduction after 50 years [5]. In the same way, Davis et al. found rising incidence within patients aged 40–44 years, from 10.7 in 1988 to 17.9 per 100 000 in 2006 [6]. Synchronous and metachronous cancers as well as a tendency of mucinous and signet ring features with a poorly differentiated histology in young adults, has been shown to present with similar features as the adult presentation [7]. In the same way, advanced stage disease of distal colon and rectum metastasizing to other organs, such as the liver, have been more commonly found in younger individuals, when compared to late-onset CRC [8].
This case shows a rare presentation of a young Hispanic patient with an EVF and histological features of early-onset advanced staged rectal adenocarcinoma. Suprapubic pain and recurrent urinary tract infections have been shown to be red flags for possible EVF in younger adults [9]. Even though the diagnosis of an EVF is hard to establish, the symptoms of suprapubic pain, pneumaturia, dysuria and tenesmus shown in this patient set the hallmarks of Gouverneur’s syndrome [9, 10]. In addition, the presence of pericolonic gas and fluid collection with a fistulous tract adjacent to the proximal rectum and the bladder help in the diagnosis.
Considering the patient’s recurrent urinary tract infections, EVF was arguably present for several months prior to his Emergency room (ER) visit. Cystoscopy and fistulography are often carried out during the onset of complications; however, in our patient it could not be performed due to the massive cancer obstruction.
Optimal treatment for EVF secondary to rectal adenocarcinoma within the Hispanic population is controversial due the complexity of the pathology and lack of reports. However, our patient’s treatment was decompressive loop colostomy for palliative care, with only two subsequent chemotherapies prior to his death.
An EVF due to an imposed rectal adenocarcinoma in a young Hispanic adult is an extremely rare pathology, which has not been reported in literature. This report provides vital information about clinical presentations of EVF secondary to rectal adenocarcinoma in a young adult without history of colorectal cancer. A special attention must be taken during clinical evaluation to ensure accurate diagnosis and early detection of colorectal cancer in the young Hispanic population. Sporadic young-onset colorectal cancer raises the question to update screening guidelines and reduce the recommended screening age to early 30s.
CONFLICT OF INTEREST STATEMENT
None Declared.



