-
PDF
- Split View
-
Views
-
Cite
Cite
Robbert-Jan Lindeman, Malin Sund, Jenny Löfgren, Trude Basso, Kjetil Søreide, Preventing spread of SARS-CoV-2 and preparing for the COVID-19 outbreak in the surgical department: perspectives from two Scandinavian countries, Journal of Surgical Case Reports, Volume 2020, Issue 5, May 2020, rjaa131, https://doi.org/10.1093/jscr/rjaa131
Close - Share Icon Share
ABSTRACT
A COVID-19 pandemic was declared on March 11 by the World Health Organization (WHO). The first cases of COVID-19 were confirmed on January 31 in Sweden and on February 26 in Norway. Despite being similar countries with universal healthcare systems, the governmental approaches to mitigation of the epidemic have varied considerably. Norway initiated a societal lockdown effective from March 12, the same day as the first confirmed death. Sweden has initiated a more laxed and gradual strategy based on the appeal for a strong personal sense of responsibility to mitigate the viral spread. In both countries, the first weeks of preparation has seen a strong reduction in elective surgery, with several implemented principles to mitigate SARS-CoV-2 spread and prepare for surgical care for COVID-19 diseases as needed. This invited leading article gives a brief overview of some of the early experiences of the outbreak in two Scandinavian countries.
INTRODUCTION
On 31 December 2019, China informed the World Health Organization (WHO) about a serious new health threat [1]. The coronavirus, SARS-CoV-2, is a virus with the potential to cause a severe and lethal pulmonary infection called coronavirus disease, COVID-19 [2]. The WHO declared the epidemic a ‘Public Health Emergency of International Concern’ on 31 January 2020 and subsequently a ‘pandemic’ on 11 March 2020. Since then, the epicenter of peak activity has moved through Europe and to North America, with several regions affected disproportionally harder than others [3].
In Scandinavia, the first cases of COVID-19 were confirmed on January 31 in Sweden, on February 26 in Norway and in Denmark on February 27. Initially, but also at time of writing, governmental approaches on how to respond to the outbreak have varied considerably. Denmark went into an effective lockdown on March 11, followed by Norway the next day (Fig. 1). Schools, universities and sporting facilities were closed, as were nurseries (with exceptions made for parents working in critical sectors of society, including doctors and nurses). The strategy of Sweden has been based on the appeal for a strong personal sense of responsibility to mitigate the viral spread, and the nurseries, kindergardens and schools are kept open. In all three Scandinavian countries, people are encouraged to work from home, and people at high risk of severe COVID-19 due to age or comorbidities are recommended to self-quarantine.
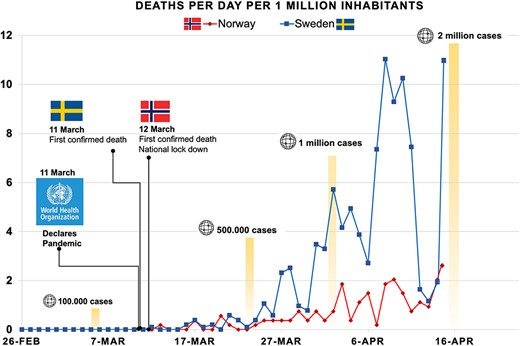
Abbreviated timeline showing some core events in Scandinavia. Legend: Core dates are depicted. Some key figures of global COVID-1p cases are depicted, reaching 2 million by 16th of April. Y-axis depicts deaths per million per country.
Despite the initial different approaches to social distancing, with aims of mitigation or suppression of the outbreak, the common primary goal has been to ‘flatten the curve’ to make it possible for hospitals to accommodate the influx of COVID-19 patients. We here briefly describe experiences from the preparation for the epidemic and change of practice in surgical departments across subdisciplines in Norway and Sweden.
EARLY VIRUS TRANSMISSION AMONG HEALTHCARE WORKERS
In Scandinavia, the criteria for SARS-CoV-2-testing have been modified during the course of the epidemic. Norway, that initially started with aggressive testing of subjects with symptoms or returning from high-endemic areas in order to get control over the spread pattern and asymptomatic COVID-19 patients, needed to restrict its activity later in March. Sweden conducted a more restrictive testing policy based on limited testing capacity.
An early effect of the initially suboptimal test routines for healthcare workers (HCW) was experienced in Norway, when one HCW returning from central Europe, was confirmed positive to SARS-CoV-2 only after having spent several days at work on the advice from the hospital. This effectively put an entire ophthalmology department in lockdown [4]. Five other HCW were infected, and more than a hundred were tested. The six COVID-19 cases were placed in home isolation, and close contact employees, students and patients were placed in home quarantine. All elective appointments were cancelled, and patients in need of urgent surgery had to be transported to hospitals in other parts of Norway.
This outbreak attracted considerable media attention, including breaking news headlines and live updates. Since this happened in late February, it likely created a public awareness and preliminary admonition to other healthcare professions. Nevertheless, a similar event happened a week later at the obstetrics unit at Stavanger University Hospital, putting about half of the obstetric department under quarantine for 2 weeks.
As an effect, any travels outside Norway were prohibited for HCW on 12th of March (Fig. 1). HCW returning from abroad were put in a 2-week self-quarantine, and the test criteria for all HCW were made more liberal. Today all HCW with fever or airway symptoms must self-isolate pending the result of a SARS-CoV-19 test. If negative, HCW must self-quarantine until the symptoms have resolved. Following the new quarantine strategy, and due to the recent winter holidays, the number of quarantined HCW was initially considerable. This effectively reduced the capacity even before the lockdown came into play.
Testing among patients and risk in hospitals
The risk of concomitant symptomatic and asymptomatic SARS-CoV-2-infection in patients undergoing surgical procedures increases by the day, yet patients are still not on a national basis, routinely tested prior to surgery. However, in the urban areas with the highest prevalence of COVID-19, such as the Oslo, Stockholm and Gothenburg regions, the hospitals are already implementing SARS-CoV-2-testing on all patients prior to surgery. As test capacity is steadily increased, a more liberal strategy for testing of patients is expected.
Preparing for the epidemic: effect on surgical activity
In both countries, surgical care has been cut to a minimum tolerable level due to the pandemic [5, 6]. Several measurements are comparable across regions (Table 1), with reorganization of healthcare processes and fast implementation of available technology, including increased use of teleconferences to manage outpatient consultations [7]. However, the scaling down of surgical activity has been done stepwise and is not uniform within countries and across regions. Like in other countries [8], most planned, elective surgery has been postponed or cancelled during the period of preparation.
| Surgical practice |
| Reduced outpatient clinical care |
| Consults/contact done by telecommunication |
| All or most elective outpatient surgery cancelled |
| Reduced or cancelled non-essential elective surgery |
| Maintained emergency and trauma capacity and essential cancer surgery |
| Staff organization |
| Reduced staff presence in clinical care; reduced doctor–nurse–patient ratios |
| Group split-up and home-based office alternating for reduced exposure |
| Minimal staff presence in meetings, e.g. MDT sessions |
| Increased use of telecommunication in meetings and/or outpatient setting |
| International travel ban (non-essential travels) for all HCWs |
| Cancelling (domestic) conferences and meetings |
| Logistics to and in hospital |
| Strict pre-hospital patient selection |
| Separate in-hospital routing for suspected or confirmed COVID-19 patients |
| Hospital centralized coordination of PPE distribution |
| Dedicated COVID-19 and non-COVID-19 surgical wards |
| Dedicated COVID-19 theater (negative pressure rooms) and recovery wards |
| Safety measures during surgery |
| Courses and simulation in PPE use and criteria |
| Increased use of PPE in emergency ward and operating theater |
| Preoperative COVID-19 screening in elective patients and in acute procedures |
| Operating theater awareness of exposure (e.g. surgical smoke formation; aerosol generating procedures; use of laparoscopy) |
| Surgical practice |
| Reduced outpatient clinical care |
| Consults/contact done by telecommunication |
| All or most elective outpatient surgery cancelled |
| Reduced or cancelled non-essential elective surgery |
| Maintained emergency and trauma capacity and essential cancer surgery |
| Staff organization |
| Reduced staff presence in clinical care; reduced doctor–nurse–patient ratios |
| Group split-up and home-based office alternating for reduced exposure |
| Minimal staff presence in meetings, e.g. MDT sessions |
| Increased use of telecommunication in meetings and/or outpatient setting |
| International travel ban (non-essential travels) for all HCWs |
| Cancelling (domestic) conferences and meetings |
| Logistics to and in hospital |
| Strict pre-hospital patient selection |
| Separate in-hospital routing for suspected or confirmed COVID-19 patients |
| Hospital centralized coordination of PPE distribution |
| Dedicated COVID-19 and non-COVID-19 surgical wards |
| Dedicated COVID-19 theater (negative pressure rooms) and recovery wards |
| Safety measures during surgery |
| Courses and simulation in PPE use and criteria |
| Increased use of PPE in emergency ward and operating theater |
| Preoperative COVID-19 screening in elective patients and in acute procedures |
| Operating theater awareness of exposure (e.g. surgical smoke formation; aerosol generating procedures; use of laparoscopy) |
The list is not intended to be exclusive but represents a core set of initiated measures.
MDT, multidisciplinary teams.
HCW, healthcare worker.
PPE, protective equipment.
| Surgical practice |
| Reduced outpatient clinical care |
| Consults/contact done by telecommunication |
| All or most elective outpatient surgery cancelled |
| Reduced or cancelled non-essential elective surgery |
| Maintained emergency and trauma capacity and essential cancer surgery |
| Staff organization |
| Reduced staff presence in clinical care; reduced doctor–nurse–patient ratios |
| Group split-up and home-based office alternating for reduced exposure |
| Minimal staff presence in meetings, e.g. MDT sessions |
| Increased use of telecommunication in meetings and/or outpatient setting |
| International travel ban (non-essential travels) for all HCWs |
| Cancelling (domestic) conferences and meetings |
| Logistics to and in hospital |
| Strict pre-hospital patient selection |
| Separate in-hospital routing for suspected or confirmed COVID-19 patients |
| Hospital centralized coordination of PPE distribution |
| Dedicated COVID-19 and non-COVID-19 surgical wards |
| Dedicated COVID-19 theater (negative pressure rooms) and recovery wards |
| Safety measures during surgery |
| Courses and simulation in PPE use and criteria |
| Increased use of PPE in emergency ward and operating theater |
| Preoperative COVID-19 screening in elective patients and in acute procedures |
| Operating theater awareness of exposure (e.g. surgical smoke formation; aerosol generating procedures; use of laparoscopy) |
| Surgical practice |
| Reduced outpatient clinical care |
| Consults/contact done by telecommunication |
| All or most elective outpatient surgery cancelled |
| Reduced or cancelled non-essential elective surgery |
| Maintained emergency and trauma capacity and essential cancer surgery |
| Staff organization |
| Reduced staff presence in clinical care; reduced doctor–nurse–patient ratios |
| Group split-up and home-based office alternating for reduced exposure |
| Minimal staff presence in meetings, e.g. MDT sessions |
| Increased use of telecommunication in meetings and/or outpatient setting |
| International travel ban (non-essential travels) for all HCWs |
| Cancelling (domestic) conferences and meetings |
| Logistics to and in hospital |
| Strict pre-hospital patient selection |
| Separate in-hospital routing for suspected or confirmed COVID-19 patients |
| Hospital centralized coordination of PPE distribution |
| Dedicated COVID-19 and non-COVID-19 surgical wards |
| Dedicated COVID-19 theater (negative pressure rooms) and recovery wards |
| Safety measures during surgery |
| Courses and simulation in PPE use and criteria |
| Increased use of PPE in emergency ward and operating theater |
| Preoperative COVID-19 screening in elective patients and in acute procedures |
| Operating theater awareness of exposure (e.g. surgical smoke formation; aerosol generating procedures; use of laparoscopy) |
The list is not intended to be exclusive but represents a core set of initiated measures.
MDT, multidisciplinary teams.
HCW, healthcare worker.
PPE, protective equipment.
The reduction in elective surgery has been performed to meet the need for increased capacity for COVID-19 patients [9, 10] but also due to insufficient storages and supplies of personal protective equipment (PPE), drugs and various other items such as disposable parts of the respirators. Another reason for scaling down on the activities has been to minimize the number of patients with no urgent needs to visit the hospitals to help prevent virus transmission to vulnerable people. In Sweden, the Stockholm region (pop. ~2 million) has had the largest number of hospitalized COVID-19 patients and deaths. Karolinska University Hospital has reduced overall surgical activity by 50%, which means that only essential surgery (cancer and emergencies) is carried out.
The surge in capacity for beds prioritized to patients with COVID-19 has also led to transformation of several departments of orthopedic surgery into alternative units. Intensive care bed capacity has been increased by expanding the areas into external units within the hospital usually reserved for perioperative care, including operating theaters, post-operative recovery and outpatient surgery units.
Currently, the consequences for surgical services are tangible. The waiting lists for ambulatory care and backlog of operations are mounting. Of concern is also the ‘silence in the acute wards,’ with lower admission rates for common disease conditions as well as some late presentation of disease conditions, potentially leading to less favorable outcomes for some patients as an added morbid effect of the pandemic. It is imminent that surgery and patients with surgical conditions is now also greatly affected as part of the global pandemic—a tangible evidence of surgery as an essential part of public health [11].
Organization of surgical care and international cooperation
The acute threat of the COVID-19 epidemic to global healthcare has led to forced reorganization of surgical care in Norway and Sweden. In high tempo hospitals have to adapt to changing circumstances, guided by current knowledge. New studies concerning COVID-19 are published ongoing, leading to multiple new global, national and local guidelines.
Surgical departments in diverse regions in Norway and Sweden are practicing somewhat different policies in terms of organization and infection prevention. However, the common goal is conducted toward minimalization of viral spread, protection of patients and operational staff and secure flow of patients within the hospital. On a general level, the organization of healthcare processes has great similarities.
In addition, the COVID-19 epidemic has accelerated effective international cooperation. Several initiatives such as the organization of a global cohort capturing real-world data concerning the management of surgical COVID-19 patients (COVIDSurg cohort study [9]) and the construction of a structured evidence-based global guideline for orthopedic management has now been established [12].
CONCLUSION
This epidemic has shown the remarkable capability of surgical departments to adapt rapidly to altering circumstances. Over the course of several weeks, the initial phases involving realization, preparing and reorganization have progressed. Now, the need for comprehensive data, international cooperation and evidence-based guidelines is essential for effective decision-making in returning to normal activity while minimizing viral spread and reducing secondary negative effects.
CONFLICT OF INTEREST STATEMENT
None declared.
Funding
None.



