-
PDF
- Split View
-
Views
-
Cite
Cite
Rickesh B Karsan, Prakash Nanjaiah, John Hogan, Dheeraj Mehta, Michael Stetchman, Concomitant aortic valve replacement and retrosternal goitre resection via mini-sternotomy: a novel case, Journal of Surgical Case Reports, Volume 2020, Issue 5, May 2020, rjaa066, https://doi.org/10.1093/jscr/rjaa066
Close - Share Icon Share
Abstract
Median sternotomy has been used to aide thyroidectomies demonstrating good outcomes; however no cases have been documented to show the use of mini-sternotomy to perform simultaneous thyroidectomy and valve surgery. We present a novel case of an 83-year-old woman with severe aortic stenosis and retrosternal goitre extending to the aortic arch deemed unsuitable for TAVI. Due to co-morbid status and anatomical position preventing routine thyroidectomy, we elected to perform a combined procedure to excise the goitre and perform an aortic valve replacement through a mini-J sternotomy, utilizing 3D-reconstructed imaging to plan our approach. This case shows that mini-sternotomy is a safe and effective method to perform concomitant thyroidectomy and aortic valve surgery.
INTRODUCTION
Large retrosternal goitres can severely complicate the approach to aortic valve surgery. Patients awaiting aortic with a large retrosternal goitre often have thyroidectomy as a separate procedure after cardiac surgery, due to significant risks posed by morbidity associated with aortic valve pathology. Usually median sternotomy has been used to aid such retrosternal thyroidectomy. Mini-sternotomy can be considered as an alternative approach for removal of large retrosternal goitres whilst minimizing the risks and complications of a full median sternotomy. In this paper, we report a unique case of concomitant left hemi-thyroidectomy with resection of its large retrosternal extension and surgical aortic valve replacement (AVR) via an upper ‘J’ mini-sternotomy.
CASE REPORT
An 83-year-old female with symptomatic (New York Heart Association Functional Classification III symptoms) critical aortic stenosis (AS), (peak gradient 105 mmHg) was admitted for elective AVR via mini-sternotomy after being found unsuitable for transcather aortic valve implantation. At pre-admission, the patient was incidentally found to have subclinical palpable thyroid goitre with tracheal deviation (Fig. 1A). A subsequent computed tomography (CT) scan showed an 8-cm paratracheal thyroid hemi-goitre, extending retrosternally and abutting the ascending aorta and arch (Figs 1B and2).
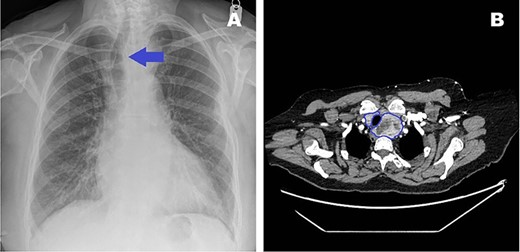
(A) Pre-admission chest radiograph highlighting visible tracheal deviation due to goitre (blue arrow). (B) Transverse CT image showing goitre relation to trachea (blue outline).
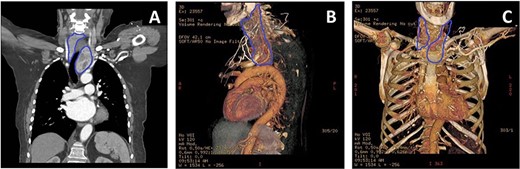
(A) CT thorax showing the extension of the retrosternal goitre (blue outline), causing tracheal deviation with extension and abutting the distal ascending aorta and arch. (B) 3D-reconstructed CT thorax lateral view highlighting goitre (blue outline) relationship with respect to ascending aorta and arch, and other mediastinal structures. (C) 3D-reconstructed CT thorax allowed planning of mini-sternotomy in relation to goitre position.
The goitre’s position would invariably make aortic cannulation and cross-clamping to perform the AVR difficult. It was deemed that the goitre needed removal first. However, the retrosternal position meant that normal cervical excision would be challenging and risky. Furthermore, due to the severe nature of the AS, she was considered unsafe to undergo thyroidectomy as a primary procedure. Endocrine surgeons were consulted and consensus dictated that combined procedure would be the best approach utilizing a mini-J sternotomy to aid in excision of the hemi-goitre prior to completing the AVR. 3D imaging was reconstructed to determine the anatomical relations in detail and plan the combined surgical approach meticulously (Fig. 2B and C).
Intraoperatively, the hemi-thyroidectomy was initiated through a 7-cm cervical Kocher incision and cervical portion of the left hemi-thyroid was mobilized after division of middle thyroid vein and thyroid artery. Based on the pre-operative imaging, a right upper ‘J’ mini- sternotomy was performed through the third intercostal space. This exposed the inferior pole of retrosternal part of the goitre and also allowed clear access to the ascending aorta, aortic arch, right atrial appendage and inferior thyroid vessels facilitating their ligation (Fig. 3A). Finally the isthmus was divided and the left hemi-goitre removed (Fig. 3B and C). The cervical incision was then packed and full-dose heparin for CPB was given. Right atrial to ascending aorta bypass circuit was now easily established. Myocardial protection was achieved with (induction) antegrade and (maintenance) direct coronary ostial intermittent cold blood cardioplegia, and routine AVR performed through a transverse aortotomy using a Perimount MagnaEase Bioprosthesis using pledgeted 2-0 ticron sutures, anchoring the prosthesis in a supra-annular position. On completion, protamine was administered and wound closure completed following a final review of haemostasis.
![(A) Intraoperative image showing hemi-goitre (blue outline) extending retrosternally [1], to ascending aorta [2] visualized via mini-sternotomy and Kocher incision. (B) Removed left hemi-goitre. (C) Post goitre removal [1], the extent of the tracheal deviation can be seen [2], through the cervical Kocher incision.](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2020/5/10.1093_jscr_rjaa066/3/m_rjaa066f3.jpeg?Expires=1773882174&Signature=E4~KJxt0LzwW9~gYZhLlJ6svtNKkwviM9KH5zkFyAdhFeRcuwyRmed44eoS0h7djJXYA0njo3OxHFSXE4ZNcYHWoFLUZhKPnsfIUeDZfouN7Kkg1qDITdl5w7TXx-MGYd-aOehPOAsCHgqyGv607U6sryz2ERt5k5-L0HqVBXK48YNLINi0VVu7HvlWtKjFdul13hiY6JFQJ9~TbgP7tVI8Ad9Q0Qs69D5swWpOKtDGiyktMoP5-fi-d1k9qi2hRVvjO1yQ67O7IXd5k4pFhDRm5qas-FFLp~saYRQ2MesIU60-2plIKBEt1jp8KeD5fbQ2KGplmI82tO2Rxf~ZCXw__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
(A) Intraoperative image showing hemi-goitre (blue outline) extending retrosternally [1], to ascending aorta [2] visualized via mini-sternotomy and Kocher incision. (B) Removed left hemi-goitre. (C) Post goitre removal [1], the extent of the tracheal deviation can be seen [2], through the cervical Kocher incision.
Post-operatively, the patient was transferred to intensive care, where recovery was uncomplicated. Minimal blood loss was witnessed from both the chest and cervical sites. All drains were removed within 48 hours and she was discharged 6 days later after an uncomplicated ward stay. She was followed up in the clinic 6 weeks after discharge with excellent outcomes and cosmesis.
DISCUSSION
We describe a patient with a history of severe symptomatic AS and incidental finding of retrosternal paratracheal hemi-goitre abutting and impeding access to the ascending aorta and arch. The anatomical relations of the goitre and its retrosternal position would make it highly difficult to perform solitary AVR and hemi-thyroidectomy. As a result, a concomitant procedure to excise the inferior retrosternal goitre and subsequent AVR was performed, facilitated by the mini-J sternotomy approach. Mini-sternotomy is now widely used in routine surgical AVR procedures with good outcomes [1].
This case addresses two areas of interest. Firstly, concomitant procedures present additional risks in cardiac surgery with bleeding being a particular concern secondary to heparinization. This case illustrates that adequate haemostasis can be achieved with correctly timed closure of a secondary surgical site. Relative timing of closure post-protamine helped to reduce the risk of post-operative cervical haematoma, by packing the cervical site.
Next, this case highlights the potential for using mini-sternotomy to aide excision of retrosternal goitres with particular use of detailed 3D imaging to plan the minimal access approach. A recent literature review has suggested that full sternotomy is successful in isolated removal of retrosternal goitres extending anteriorly into the mediastinum [2]. Nankee et al. suggested in a retrospective review that use of sternotomy for thyroidectomy is largely required when the goitre extends to and below the aortic arch [3]. With the move towards more minimally invasive approaches in cardiac surgery, there is potential for the use of mini-sternotomy as a viable alternative to full sternotomy in concomitant cases.
We support the use of mini-sternotomy for the safe removal of retrosternal thyroid goitres extending to the ascending aortas and aortic arch. In cases where goitres would impede safe access for AVR, we feel that joint procedures are a practical option with proper planning to reduce bleeding.
CONFLICT OF INTEREST STATEMENT
None declared.



