-
PDF
- Split View
-
Views
-
Cite
Cite
Jeremia J Pyuza, Alice A Andongolile, Christain E Issangya, David Msuya, James J Yahaya, Elichilia R Shao, Alex R Mremi, Missed opportunity of deworming a Maasai boy from nomadic family leading to life threatening intestinal obstruction, Journal of Surgical Case Reports, Volume 2020, Issue 5, May 2020, rjaa096, https://doi.org/10.1093/jscr/rjaa096
Close - Share Icon Share
Abstract
Mass deworming against soil-transmitted helminthiasis, including Ascaris lumbricoides (AL), is one of the largest public health interventions in low- and middle-income countries. The prevalence of A. lumbricoides in Tanzania is 6.8%. We present a 3-year-old male of a known Tanzanian nomadic tribe (Masaai tribe) with history of missed deworming, who was brought to the emergency department with a 3-day history of constipation, nonprojectile, bilious vomiting, generalized abdominal distension and pain.
He was diagnosed with intestinal obstruction by the use of a plain abdominal X-ray, which revealed marked gaseous distension of the stomach and bowels without significant air-fluid levels. He was initially treated with intravenous ceftriaxone 50 mg/kg, metronidazole 15 mg/kg and acetaminophen 15 mg/kg. An explorative laparotomy was then performed. Intraoperative findings demonstrated a dense collection of A. lumbricoides worms in the gangrenous proximal jejunum and duodenum. Thorough abdominal lavage was carried out and abdomen was closed.
INTRODUCTION
Mass deworming against soil-transmitted helminthiasis, including Ascaris lumbricoides, is one of the largest public health interventions in low- and middle-income countries (LMIC) [1]. Infection of the intestinal nematode, A. lumbricoides is one of the most common human helminth infections [2]. Ascaris lumbricoides infects 0.8–1.2 billion people worldwide, with a high prevalence in tropical and subtropical areas [3]. It is estimated that 73% of infected individuals are found in LMIC [4]. The overall incidence of A. lumbricoides infestation in sub-Saharan Africa is 16% [9]. Schule et al. report the prevalence of A. lumbricoides infestation in Tanzania to be 6.8% and attributes the warmth and wet climate that favors year-round transmission [10].
The primary modes of A. lumbricoides transmission occur via ingestion of A. lumbricoides eggs secreted in human feces, which subsequently embryonate in the soil and contaminate food/water sources, or by consuming the raw meat of an infected pig or chicken [5]. Symptomatic cases typically occur in those with high worm burden and manifest with abdominal discomfort, pneumonitis and anorexia [4]. Left untreated, ascariasis may result in lethal complications such as intestinal obstruction, pancreatic damage, malnutrition, growth retardation and peritonitis [6]. Overall mortality caused by A. lumbricoides is reported to be very low. However, ascariasis has enormous health and social implications for school aged children, especially in LMIC, such as a decrease in school performance and permanent disability.
AL complications are preventable through well-organized deworming programs in areas of high infection prevalence. In 2017, the World Health Organization (WHO) produced recommendations for prevention of soil-transmitted infections including improvement in sanitation, health and hygiene behaviors like hand washing, footwear and use of toilets. For preschool and primary school children, the WHO recommends one- or two deworming treatments depending to the prevalence of disease. These interventions remain to be a major challenge especially in nomadic populations [7–8]. Worldwide, the prevalence of deworming among preprimary school children in endemic areas is low [1]. As a result, patients in LMIC may present with later sequelae of A. lumbricoides infections.
CASE PRESENTATION
A 3-year-old male of a known Tanzanian nomadic Masaai tribe was brought to the emergency department with a 3-day history of constipation, nonprojectile, bilious vomiting, generalized abdominal distension and pain. His mother denied any history of deworming. His past medical and family history was unremarkable. On physical examination, the child was pale, weak with an altered level of consciousness, Glasgow Coma Score of 12/15 and febrile with a body temperature of 37.9°C. His blood pressure was 112/70 mm Hg with a pulse rate of 90 beats/min. The patient’s abdomen was distended and tender with guarding and dullness to percussion. Laboratory investigations revealed hemoglobin of 9.2 g/dl (12.0–16.0) with normal white blood cells. A plain abdominal X-ray revealed marked gaseous distension of the stomach and bowels without air-fluid levels (Fig. 1). Similar findings were observed in the abdominal ultrasound scan.
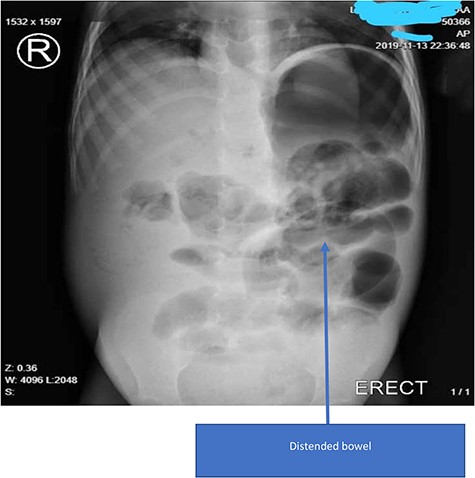
Plain X-ray of the patient showing gastrointestinal distention without air-fluid levels or ‘railway tracks’.
Based on the clinical and physical examination findings, a working diagnosis of intestinal obstruction with peritonitis was made. Further investigations such as a computed tomography scan were not possible due to financial constraints. The patient was admitted and rehydrated with 2.0 L of ringer lactate (RL) alternated with dextrose normal saline. He was treated with intravenous ceftriaxone 50 mg/kg, metronidazole 15 mg/kg and acetaminophen 15 mg/kg. An explorative laparotomy was performed. Intraoperative findings demonstrated volvulus of the terminal ileum with gangrenous changes of the small intestine ~48 cm from the ileoceacal junction. A dense collection of A. lumbricoides worms in the gangrenous proximal jejunum and duodenum (Fig. 2) accompanied by 1500 ml of foul-smelling peritoneal fluid was found.
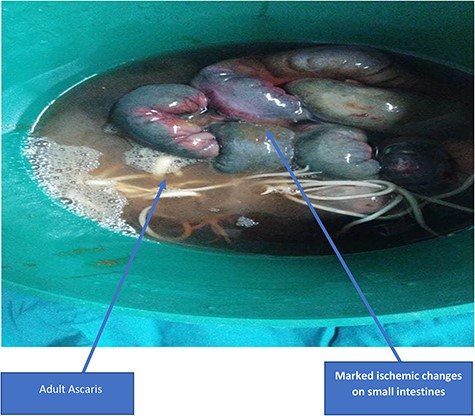
Marked ischemic changes of the small bowel with adult A. lumbricoides worms protruding from the bowel.
Resection of the gangrenous portions of the bowel was performed with extraction of the A. lumbricoides worm collection (Fig. 3). An ileotransverse end-to-side anastomosis was then carried out. On microscopic examination slide showed A. lumbricoides on the sampled small bowel segment stained with hematoxylin and eosin (H&E) (Fig. 4). There was also an aggregation of lymphocytes forming granulomatous lesions with central necrosis (Fig. 5).
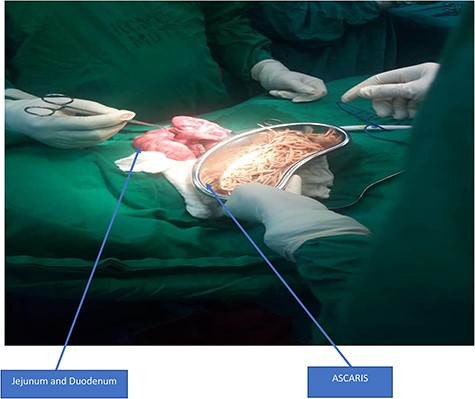
Extraction of A. lumbricoides from jejunum and duodenum by enterotomy.
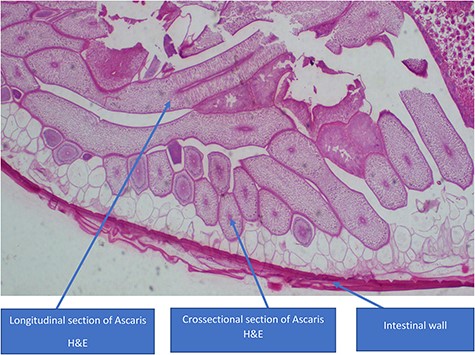
Showing A. lumbricoides on the sampled small bowel segment stained with H&E.
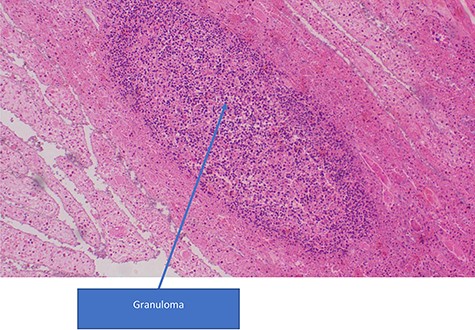
Infiltration of lymphocytic inflammatory cells with aggregation to form a granuloma in a necrotic tissue (H&E stains, ×100).
Postoperative management involved intravenous fluid 1.5 L of RL alternated with dextrose lactate solution. Intravenous ceftriaxone 50 mg/kg once a day, metronidazole 15 mg/kg every 8 h for 5 days, intramuscular pethidine 25 mg every 8 h for 1 day and a single dose of orally albendazole 400 mg. Postoperative period was uneventful and he was discharged 6 days following operation. We followed up the child for 4 months postdischarge and his condition remained stable with resumption of normal bowel function.
DISCUSSION
Prevention and treatment of A. lumbricoides infections in rural and remote populations including the Tanzanian Masaai tribe continue to pose a challenge for healthcare providers. Although the Tanzania policy for once yearly deworming program for primary school and preprimary school children continues to be enacted, this does not necessarily reach all infected population. Rural and remote populations continue to experience barriers to routine and preventative care such as lack of reliable transportation, awareness of medical treatment and presentation and infrequent communication with medical care providers.
In this case, the child had several known risk factors for worm infestation, yet he was never taken to a clinic for deworming. It is important to consider distance to the nearest treatment facility, which was ~200 km. The relative lack of resources in this patient’s case likely contributed to failed adherence to antenatally early deworming program and lack of timely diagnosis leading to detrimental complications of intestinal obstruction and severe anemia.
In Tanzania, children are entitled to receive necessary supplements and other interventions such as routine vaccines. Due to factors like remote populations, lack of community awareness and constant movements of family in search for animal pastures, certain children miss the opportunity to utilize their basic right of health care. The government of Tanzania attempts to address these barriers by offering mass treatment via mobile treatment camps; however, this temporary measure does not necessarily reach all infected population. Knowing how remote populations and special groups of people can most effectively be treated with deworming therapy is an important strategy to prevent occurrences of severe A. lumbricoides sequelae in Tanzania.
References
- ceftriaxone
- acetaminophen
- constipation
- ascaris lumbricoides
- developing countries
- dilatation, pathologic
- emergency service, hospital
- gangrene
- helminthiasis
- intestinal obstruction
- intraoperative care
- irrigation
- metronidazole
- pain
- abdominal radiography
- soil
- tanzania
- abdomen
- duodenum
- jejunum
- public health medicine
- stomach
- abdominal swelling
- air fluid level
- laparotomy, exploratory
- vomiting bile



