-
PDF
- Split View
-
Views
-
Cite
Cite
Jhony Alejandro Delgado Salazar, Natalia Carolina Naveda Pacheco, Paola Alexandra Palacios Jaramillo, Santiago Danilo Garzón Yépez, Victor Rafael Medina Loza, Carlos Alberto Romero Alvarado, Bernabé Esteban Aguilar Ayala, Gabriel Alejandro Molina, Ingestion of razor blades, a rare event: a case report in a psychiatric patient, Journal of Surgical Case Reports, Volume 2020, Issue 5, May 2020, rjaa094, https://doi.org/10.1093/jscr/rjaa094
Close - Share Icon Share
Abstract
Foreign body ingestion is a common condition in clinical practice, thankfully most of the cases do not require any surgery as most foreign bodies can pass through the bowel without injuring it. Treatment depends on the size and kind of foreign bodies. When complications arise, patients may require urgent medical attention. Self-harm by sharp foreign body ingestion is a rare event that must always be promptly treated and should always be prevented. Psychiatric patients and inmates are the most affected population. A high index of suspicion is required to treat this rare condition, which may be preventable if there is adequate mental and medical therapy along with close monitoring and family support. We present the case of a 31-year-old psychiatric patient. After prompt treatment, two razor blades were surgically removed from her intestines. She fully recovered and is doing well on follow-up controls.
INTRODUCTION
Foreign body ingestion is a common condition in children and a rare one in adults; when it occurs, it is more frequently seen in prison inmates and psychiatric patients [1, 2]. Treatment in these patients is extremely complex; therefore, a multidisciplinary team is required to prevent this rare but life-threatening situation [1, 3]. When a sharp object like a razor blade is ingested, prompt treatment is vital as complications can cause severe morbidity or mortality. When dealing with these patients, the long-term objective is patient safety, and therefore, close follow-up along with medical therapy is of paramount importance [1, 4]. We present the case of a 31-year-old psychiatric patient; she ingested two razor blades that required urgent surgery. She fully recovered and is doing well on follow-ups.
CASE REPORT
The patient is a 31-year-old female with a past medical history of cholecystectomy, appendectomy, depression, substance abuse (alcohol), and suicide attempts. She was on psychiatric therapy and anti-depressive drugs. Nonetheless, during the past year, her medical controls became increasingly irregular, her psychiatrist was relocated, and it was difficult for her to attend the appointments. Two weeks before arriving at the emergency room and after her father passed away, she experienced a major depressive episode. These symptoms combined with a lack of adequate therapy led her to ingest two razor blades. 48 hours after this incident, she presented with acute abdominal pain, nausea, and bloody stools; thus, she was brought immediately by her family to the emergency room.
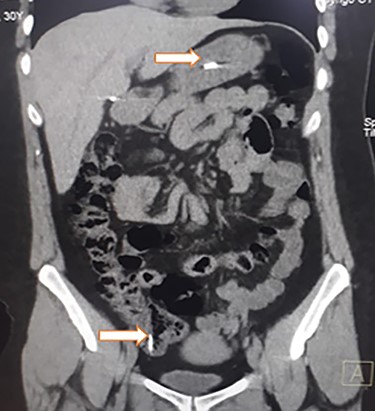
Abdominal CT, revealing two metal bodies, one in the stomach and one in the cecum.
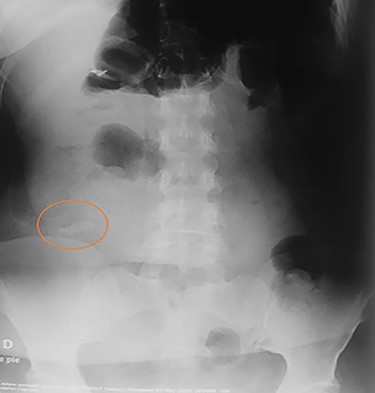
On clinical examination, a dehydrated and tachycardic (112 bpm) patient was encountered, she had diffuse pain in her lower abdomen without tenderness. After reanimation, an abdominal X-ray found two metal bodies in the bowel (Fig. 1); therefore, a computed tomography (CT) was requested, which revealed two metal foreign bodies, (razor blades) one in the stomach and one in the cecum without pneumoperitoneum (Fig. 2). As the patient did not have any tenderness, an upper endoscopy and colonoscopy were planned. During the upper endoscopy, the razor blade was detected in the antrum and was embedded in the mucosa (Fig. 3). After several failed attempts to remove the foreign object, the procedure was interrupted due to a risk of inadvertent perforation, and surgery was decided.
On laparotomy, the stomach, small bowel, and colon appeared normal without any lacerations, the two razor blades were identified and a 3 cm gastrostomy was done removing the first razor blade without complications; after this, a 3 cm colotomy was done in the ascending colon along the taenia coli and the second razor blade was removed, the colotomy and gastrostomy were sutured in a two-layer fashion with an absorbable suture and the procedure was completed without complications.
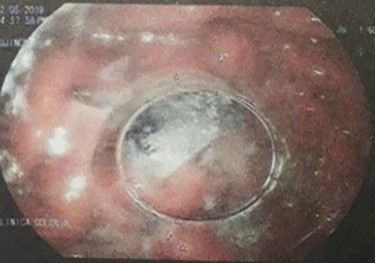
Upper endoscopy, the razor blade is seen embedded in the mucosa.
Her postoperative period was uneventful (Fig. 4); liquid diet was started on the second postoperative day and was followed by a full diet. A complete psychiatric evaluation was requested before discharge, and she was kept on close surveillance for a year. On follow-ups, the patient is doing well and is still under psychiatric surveillance and anti-depressive medication.
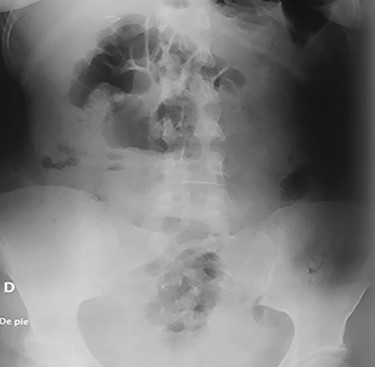
Abdominal X-ray on the postoperative period without any razor blades.
DISCUSSION
Ingestion of foreign bodies is a common condition in general practice. This scenario is mostly accidental and happens regularly in children [1]. Intentional ingestion of foreign bodies usually happens in prisoners to achieve hospitalization or as a suicide purpose. The motivation behind this event is often manipulative, depressive or psychiatric [1, 2]. Self-ingestion of a foreign body as a suicidal purpose is rare because it is painful; it takes a long time to end with dead and most cases ineffective, and hence, the victim usually opts for other suicide methods [3, 4]. When a suicide victim ingests foreign bodies, they are usually pins, cylindrical button batteries, small pocketknives, dentures, sponges, coins or razor blades [1, 3], as it was discovered in our patient.
Large, round objects such as coins get trapped on the thoracic inlet or the gastroesophageal junction; when sharp objects are ingested, they are usually trapped at areas of anatomical narrowing such as the duodenal loop, ileocecal valve, in areas near intestinal adhesions, abdominal tumors, hernias or intestinal resections. Perforations usually happen in these areas [1, 3, 4]. In our patient, thanks to a prompt intervention, the razor blades were removed without any complications. Small objects (diameter less than 2.5 cm and length less than 6 cm) will usually transit through the small intestine and the majority will pass spontaneously (80%) within a week, nonetheless, any foreign object (especially thin, stiff, sharp, long, pointed, and metallic) could be a potential cause of perforation and may cause delayed complications such as peritonitis, fistula, adhesion and abscesses [1, 5].
When approaching an ingested foreign object, the first approach should be endoscopic to try to remove the foreign body, and if it fails and there’s is a high risk of perforation, surgery should not be delayed [1, 6, 7]. In our patient, the endoscopy failed and due to the evidence of two razor blades, surgery was decided.
If a perforation occurs, the foreign object may lie in the bowel lumen close to the site of perforation, it can be found free in the peritoneal cavity or it could fall back into the bowel lumen and migrate distally to perforate it again or pass [4, 7]. Symptoms of perforation by foreign objects are nonspecific and can mimic other causes of abdominal pain, including diverticulitis, appendicitis, ureteric colic, inflammatory masses, and gynecologic conditions, among others [1, 8]. In our patient, she experienced abdominal pain, nausea, and bloody stools.
The management of intentional foreign body ingestion in the psychiatric population is complex, not only because cooperation from these patients is difficult but because they can have potentially lethal behaviors that need rapid medical attention. The role of the medical team and family support is critical when approaching these patients. Medical, pharmacological and cognitive-behavioral interventions are necessary to achieve the long-term objective of patient safety.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
FUNDING
None.



