-
PDF
- Split View
-
Views
-
Cite
Cite
Nikolaj Travica, Karin Ried, Andrew Pipingas, Irene Hudson, David Young, Andrew Scholey, Avni Sali, The effects of knee arthroplasty on plasma vitamin C concentrations and cognitive function: a case study, Journal of Surgical Case Reports, Volume 2020, Issue 5, May 2020, rjaa111, https://doi.org/10.1093/jscr/rjaa111
Close - Share Icon Share
Abstract
Post-operative neurocognitive disorders are becoming well-documented conditions, with their pathogenesis remaining unclear. Vitamin C is a molecule that has recently demonstrated both a potential link with cognitive function and a significant post-operative decline. Here, we present a case study of a 72-year-old male who underwent total knee replacement surgery. The patient demonstrated a substantial decline in plasma vitamin C concentrations, indicative of a severe deficiency, during the first post-operative week (post-operative Days 3 and 7). Similarly, at these time points, a number of validated paper and pen tests revealed a substantial decline in cognition on tasks relating to total recall, delayed recall, motor speed, recognition and motor speed, with no signs of delirium. These results provide the justification for larger, cohort studies to determine whether post-operative plasma vitamin C depletions could contribute to cognitive deficits post-operatively.
INTRODUCTION
Post-operative neurocognitive disorders are common post-operative complications, particularly effecting geriatric patients post-operatively. The most common symptoms can be loosely categorized into post-operative delirium (acute confusion and disorientation) and post-operative cognitive dysfunction (persistent post-operative cognitive decline determined through cognitive assessment) [1]. Despite the severity of these symptoms, the pathogenesis and contributing factors still remain unclear [1].
Humans make up the handful of species that are unable to biosynthesize the water-soluble molecule, vitamin C. The vitamin’s involvement in a number of biological functions, including support of the central nervous system, has been recently recognized [2]. Systematically higher plasma vitamin C concentrations have been observed in cognitively intact participants as opposed to cognitively impaired ones, who often display inadequate/deficient plasma vitamin C concentrations (<28 μmol/L) [3]. Additionally, our recent study using healthy adults revealed a significant, positive association between plasma vitamin C and a series of paper and pen tests alongside a computerized cognitive battery [4].
Studies have routinely demonstrated a significant decline in post-operative plasma vitamin C concentrations, representative of inadequate/deficient concentrations [5]. However, a majority of these have only assessed plasma concentrations within the first post-operative week and have failed to investigate whether there is a possible link between post-operative vitamin C concentrations and the emergence of pathophysiologies.
To date, this is the first case report to investigate whether post-operative changes in plasma vitamin C concentrations may be associated with post-operative cognitive decline.
CASE REPORT
We report a case of a 72-year-old male with early lateral compartment osteoarthritis of the right knee, experiencing degenerative tear of the right meniscus. The patient had significant synovitis, medial compartmental pain and increasing weakness in the right knee. He presented with well-controlled hypertension and possible type 2 diabetes mellitus. The patient displayed no history of psychiatric disorders. They ceased taking a majority of supplements 2 weeks prior to surgery, continuing oral vitamin C (500 mg, twice daily) until 24 hours pre-surgery. The patient underwent a right triathlon/titanium total knee replacement with patella resurfacing (Fig. 1), utilizing Stryker precision navigation with a tourniquet release time of 8 minutes. Spinal anaesthetic with 20 μg/kg of fentanyl was used.

X-ray of patient’s knee following the total knee replacement with patella resurfacing.
The Modified Mini Mental State Examination (3MS) confirmed no major neurocognitive disorder/dementia prior to the surgery. The patient primarily had their plasma vitamin C concentrations tested alongside validated paper- and pen-based cognitive assessments 7 days prior to surgery, during the first post-operative week (Days 3 and 7) and 1, 3 and 6 months following surgery.
Further assessments during these time points included dietary nutritional intake of vitamin C alongside a range of other nutrients, serum vitamin B12 concentrations, cardiovascular biomarkers, sleep quality, pain and mood. Plasma vitamin C concentrations at each time point are displayed in Fig. 2.
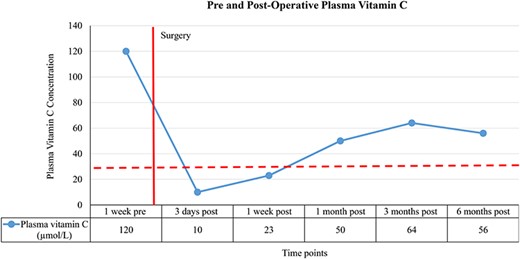
Red line represents timing of surgery, dotted line represents divide between inadequate/deficient and adequate plasma vitamin C concentrations, <28 μmol/L = inadequate/deficient, ≥28 μmol/L = adequate, pre = pre-surgery and post = post-surgery.
A profound decline in plasma vitamin C concentrations was primarily observed on the third (−92%) and seventh (−81%) post-operative days, representative of substantial deficiency. Concentrations reached adequate levels and remained in this range during the 1, 3 and 6 month post-operative assessments.
Post-operative 3MS scores revealed no signs of dementia or delirium (score: 94/100, no signs of confusion or disorientation). Additional, more sensitive pre- and post-operative cognitive scores are displayed in Fig. 3.
![(A–C) Measures derived from the Hopkins Verbal Learning Test-Revised [9], delayed recall/recognition index scored out of 12 points; total recall scored out of 36 points, Symbol Digit Modalities Test [10] assessed psychomotor speed, attention, visual scanning, highest score is 110 points, red line represents timing of surgery and post = post-surgery.](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2020/5/10.1093_jscr_rjaa111/2/m_rjaa111f3.jpeg?Expires=1774103136&Signature=PQ9bossPT63h9gWgV3X5sire6fMvbYon--hGK3YFrinVuVEv4V6zRblV3QE97LCGofnd6r29xqjk64nCK6Mk-Qbt~cfdEmhqLUNdGZQ~ndSxOKsOkJaJr3WM67fUudVsORoacMGj9XISEsGOcLVeuyEdRCrz0BXWFWz-bMiUyYCBQHfqocFfi8LOUfl6KNzuV~kxB3fVmvR9Z6Tq8MO-cosIMojcErNJU4l4Dc~-tunukqJmQrTbI7AOS3WS9hCCxmV99EG6JQ6wpb3hRs~md4rzcA8q-4ai8u0~ZSMT0nteBNkWOChYOxTsfkca~j1W5hTrW8mMr8e~BQ3LUQkqPw__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
(A–C) Measures derived from the Hopkins Verbal Learning Test-Revised [9], delayed recall/recognition index scored out of 12 points; total recall scored out of 36 points, Symbol Digit Modalities Test [10] assessed psychomotor speed, attention, visual scanning, highest score is 110 points, red line represents timing of surgery and post = post-surgery.
A large decline was observed in total recall, delayed recall, recognition and SDMT scores (testing for divided attention, visual scanning and psychomotor speed) on the third and seventh post-operative days. Scores stabilized during 1, 3 and 6 months post-operatively.
Serum vitamin B12 concentrations remained consistent and within normal ranges during all testing sessions. The patient’s average intake of vitamin C (2 weeks prior) was within the recommended daily intake (100 mg/d) 1 week before surgery (average intake: 130 mg/d vitamin C) and at all post-operative testing points. The patient continued supplementing on vitamin C until 24 hours prior to surgery. Consistencies between pre- and post-operative dietary intake of various minerals and vitamins were observed. Mood, sleep and pain assessments indicated no changes post-operatively.
The patient was discharged on the fourth post-operative day, the discharge summary revealing no additional comorbidities, including no electrolyte imbalances, major infections or malnutrition. During the post-operative period, the patient was prescribed medication for reflux, thyroid function, blood sugar levels, a blood thinner, analgesic and prophylactic antibiotics (initial 24 hours).
DISCUSSION
Our results demonstrated a substantial decline and severe deficiency in plasma vitamin C concentrations during the first post-operative week. This decline was paralleled by a decline in cognitive performance on tasks involving total and delayed recall, recognition, divided attention and motor speed during the first post-operative week. No signs of delirium were apparent.
Consistent with previous studies, vitamin C concentration substantially dropped during the first post-operative week [5] and concentrations below 28 μmol/L were associated with noticeably lower cognitive performance [4]. Although it has been proposed that symptoms of vitamin C deficiency develop following weeks of vitamin C depletion [6], the sudden and prominent decline in this case may have compromised cognitive function, interfering with the vitamin’s homeostasis within the CNS.
Additional biomarkers that were assessed by the surgical team and the patient’s GP revealed increases in C-reactive protein, white blood cells (neutrophilia) and blood sugar levels during the first post-operative week. It is known that neutrophils have a high affinity for vitamin C from plasma [7] and that glucose may interfere with the vitamin’s cellular absorptive/recycling capacity [8]. Therefore, these factors may have contributed to the vitamin C and/or cognitive depletion. Additionally, the concoction of newly administered post-operative medications may have had an effect on either of the outcome measures.
Our research team is proposing to conduct a larger, cohort study that will clarify these observations and better determine whether there is a potential link between post-operative cognitive decline and depletions in plasma vitamin C concentrations. A computerized cognitive battery capable of assessing additional cognitive domains will also be incorporated [4]. Overall, based on this case study, there may be a possible association between post-operative plasma vitamin C depletion and a cognitive decline, particularly during the first post-operative week.
EXPERIMENTAL ETHICS
Written consent was obtained from the study participant. The study protocol has been approved by multiple Human Research Ethics Committees.
CONFLICT OF INTEREST STATEMENT
None declared.



