-
PDF
- Split View
-
Views
-
Cite
Cite
John M Le, Sherry S Collawn, Revisiting the value of the ‘bandoneon’ flap for lower lip reconstruction: a report of two cases and outcome, Journal of Surgical Case Reports, Volume 2020, Issue 5, May 2020, rjaa082, https://doi.org/10.1093/jscr/rjaa082
Close - Share Icon Share
Abstract
Mild- to moderate-sized lip defects that affect one- to two-thirds of the total lip length often require that utilization of local soft tissue rearrangement in order to re-establish lip anatomy, function and esthetics. The use of local flaps in lip reconstruction often follows oncologic resection of common skin malignancies including basal cell carcinoma and squamous cell carcinoma. When considering the types of flaps to use for lip defects of one- to two-third total length, a variety of flaps designs have been described, each with its benefits in drawbacks. In this article, we reintroduce the use and value of the bilateral mucomyocutaneous ‘bandoneon’ flaps for lower lip reconstruction in two of our patients. When compared with other flap designs, it can be used as a single-stage procedure with a very good esthetic outcome, minimal to no microstomia and preservation of lip competence and sensory function.
INTRODUCTION
Lip defects resulting from trauma or ablative surgery can pose a challenging task for a reconstructive surgeon. Many surgical techniques have been described and utilized based on size and location of the lip defect [1]. Even with the many techniques described in the literature, reconstructive surgeons continue to revise, modify and develop new techniques to improve esthetic and functional outcome.
Lip reconstruction is most commonly used in oncology cases. Skin cancer is the most common malignancy occurring in the USA and worldwide. In particular, the leading two types of skin cancers are basal cell carcinoma and squamous cell carcinoma [2]. Approximately 90% of non-melanoma skin cancers occur due to prolonged exposure to ultraviolet (UV) radiation from the sun [3]. When focusing specifically on lip cancers, basal cell carcinoma has been shown to be more prevalent on the upper lip and squamous cell carcinoma on the lower lip, both of which are commonly exposed to UV radiation. Furthermore, almost 90% of lip cancers occur in the lower lip with squamous cell carcinoma being the most common histologic variant, followed by basal cell carcinoma [4]. Fortunately, with early detection and treatment, surgery is the curative treatment for basal and squamous cell carcinoma. A wide local excision of the tumor with 5–10 mm circumferentially is the standard procedure performed [5–7]. As a result, this often leaves a considerable sized defect that can be challenging to close primarily without distorting the local soft tissue anatomy and potentially creating a limited mouth opening (microstomia). Often with lip defects of one- to two-thirds out of the total lip length, the use of local advancement flaps results with better esthetic outcome due to the utilization of the remaining lip structure.
In this article, we aim to reintroduce the use and value of the stretched mucomyocutaneous ‘bandoneon’ flap that was previously described by Peled et al. for lower lip reconstruction [8–10]. When compared with other techniques, this technique offers a good esthetic outcome with minimal scarring, preservation of lip competence and sensory function and minimal microstomia.
FLAP DESIGN
After resection of the tumor with clear margins confirmed with frozen section analysis, ensure that there is adequate hemostasis on the tissue bed of the defect area. At the inferior portion of the defect site, extend a horizontal line in a zigzag design bilaterally from the wound edges. Make sure that this line does not go beyond the labiomental junction. A full-thickness incision is then completed through the skin, muscle and oral mucosa with careful attention for the inferior labial arteries laterally as the flaps are raised. The flaps are then stretched medially to cover the defect with the points of the zigzag approximated appropriately. The flaps are then sutured in a three-layered fashion: mucosa, muscle and skin (Fig. 1).
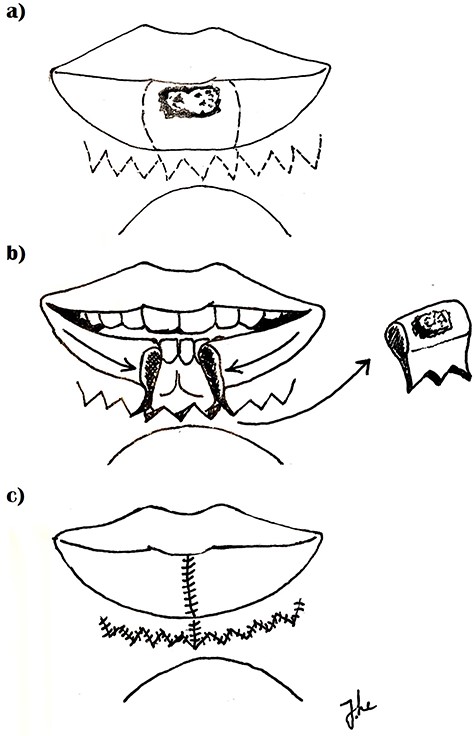
Flap design (a) incision marked (b) specimen excised, flap medially advanced (c) closure.
CASE SERIES
Two white male patients presented with squamous cell carcinoma of the lower lip that were surgically excised and the defect reconstructed using bilateral ‘bandoneon’ advancement flaps. Both received wide local excisions with negative margins prior to reconstruction. The first patient underwent both surgical excision followed by reconstruction in one stage, whereas the second patient first underwent surgery and reconstruction in two stages due to the defect size.
Case 1
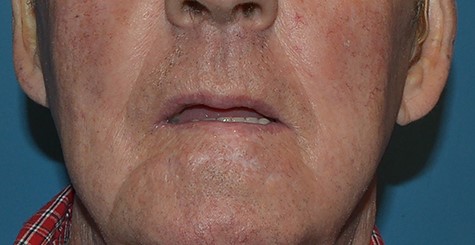
A 75-year-old male presented with a moderately differentiated invasive squamous cell carcinoma affecting one-third of the lower lip length (Fig. 2). A wide local excision with negative margins was performed and resulted in a 5- × 3-cm defect. Using the zigzag or ‘running W’ incision design in the labiomental fold, bilateral mucomyocutaneous ‘bandoneon’ flaps were raised based off of the inferior labial arteries (Fig. 3). The flaps were then advanced medially, intercalating the points and troughs of the incision line appropriately. Closure was then achieved in a sequential three-layered fashion starting with the orbicularis oris muscle fibers, mucosa, and skin, respectively. Most importantly, the wet line and vermilion border must be realigned properly. Vicryl sutures were used for the muscle layer, chromic gut sutures for mucosa and nylon sutures for the skin. At the 18-month follow-up appointment, physical examination revealed a well-healed and camouflaged scar, no microstomia, preserved lip sensation and lower lip competence. The patient was very pleased with the esthetic outcome (Fig. 4).

Squamous cell carcinoma of the lower lip affecting central lip.

Lower lip defect after surgical excision with zigzag flap design drawn.
Case 2
A 48-year-old male presented with an invasive squamous cell carcinoma involving two-thirds of the lower lip (Fig. 5). Tumor resection and reconstruction was planned in two stages due to the initial size of the tumor. In the first stage, a wide local excision was carried out with negative margins observed via frozen sections (Fig. 6). Then a dermal repair scaffolding (Integra® PriMatrix®, Integra LifeSciences, Plansboro, NJ, USA) was used for space maintenance and tissue bed preparation (Fig. 7). At the 1-week follow-up appointment, final pathological permanent sections verified negative margins, and the patient was scheduled for the second stage of the surgery.

Squamous cell carcinoma of the lower lip affecting the midline to left commissure.


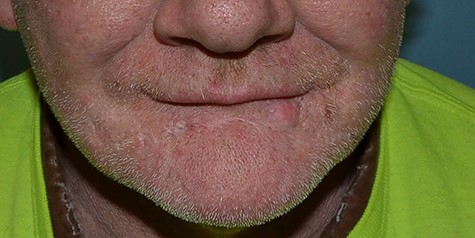
At the time of reconstruction, the size of the defect was 2.5 × 10.5 cm after removal of the dermal scaffold. Similar to the first case, bilateral mucomyocutaneous flaps were raised in addition to a buccal rotational flap for the advancement of the vermilion at the left lateral commissure. A back-cut incision was performed in the mucosa on the flap raised on the left in order to advance the buccal mucosa anteriorly (Fig. 8). A three-layered closure was used in similar fashion as previously described with vicryl sutures for the muscular layer, chromic gut for mucosal layer and nylon suture for the skin (Fig 9). At three-month follow-up, the surgical site was well healed with notable thinning of vermillion border of the lower lip and a small scar contracture of the inner buccal mucosa. The patient did not report any difficulty with speech, eating or microstomia. The patient underwent a revision surgical procedure with a V-Y advancement for the remaining cutaneous ‘notch’ of the functional lower lip, Z-plasty for scar contracture of inner buccal lower lip and abdominal fat grafting to the lower lip. At the 14-month follow-up appointment, the patient continues to report no problems with speech, oral function or microstomia (Fig. 10).


DISCUSSION
Lip reconstruction after tumor resection can be challenging due to the size of the full-thickness defect and its effect on local tissue anatomy, esthetics and function. In addition to the commonly performed local flaps that have been described in the literature for defect sizes of one- to two-thirds of the total lip length, we reintroduce the use and value of the bilateral mucomyocutaneous ‘bandoneon’ flap for lower lip reconstruction. Whether performed in a single or delayed stage, this technique has demonstrated good esthetic outcome with minimal scarring, preservation of lip competence and sensory function and minimal microstomia. On the other hand, other techniques may result in larger scars, denervated flaps and significant microstomia. All in all, based on the size and location of the defect, lip reconstruction can be performed using a variety of surgical techniques, each with their own benefits and drawbacks. We hope that by reintroducing the ‘bandoneon’ flap, reconstructive surgeons will remember to keep this technique in their armamentarium for the future.
CONFLICT OF INTEREST STATEMENT
None declared.
References
http://www.cancer.org/cancer/skincancer-basalandsquamouscell/detailedguide/skin-cancer-basal-and-squamous-cell-what-is-basal-and-squamous-cell , (9 February 2020 date last accessed).



