-
PDF
- Split View
-
Views
-
Cite
Cite
Roberto Bustos, Michail Papamichail, Alberto Mangano, Valentina Valle, Pier Cristoforo Giulianotti, Robotic approach to treat Median Arcuate Ligament syndrome: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 5, May 2020, rjaa088, https://doi.org/10.1093/jscr/rjaa088
Close - Share Icon Share
Abstract
The Median Arcuate Ligament (MAL) syndrome is the symptomatic compression of the celiac trunk by the MAL and other ganglionic periaortic tissue. Despite its rarity, this condition is significant from a clinical, diagnostic and management standpoint and it is usually a diagnosis of exclusion. A 61-year-old female with history of intermittent postprandial epigastric pain was diagnosed with MAL syndrome during CT scan imaging (no other causes of pain were identified). Patient successfully underwent robotic MAL release with symptoms improvement after surgery. The robotic approach is feasible and may allow a very precise and delicate dissection with release of the MAL.
INTRODUCTION
The Median Arcuate Ligament (MAL) is a diaphragmatic fibrous arch connecting the crura and forming the aortic hiatus. It is hypothesized that the compression of the celiac trunk by the MAL and other ganglionic periaortic tissue causes the MAL syndrome [1]. It has been proposed that 10–24% of the population have certain degree of compression of the celiac artery [2]. Nevertheless, this finding is clinically significant only in a small subgroup of patients [1]. In case other conceivable causes for the abdominal symptoms have been ruled out, the patient may benefit from a surgical decompression [3].
Minimally invasive techniques, especially a robotic approach, may offer superior accuracy during the dissection maneuvers and potentially can provide a more effective release of the MAL [4].
CASE PRESENTATION
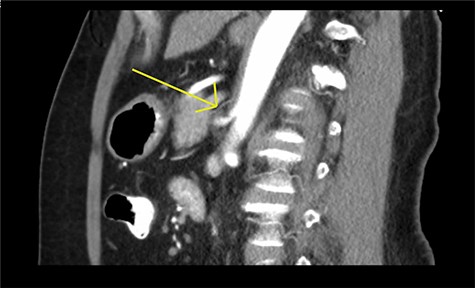
A 61-year-old female presented with a 1 year history of intermittent epigastric pain worsened by eating, nausea and diarrhea. She had a past medical history of hypertension, irritable bowel syndrome and GERD. CT imaging revealed celiac artery stenosis and a possible MAL syndrome (Fig. 1). No other causes were identified (normal EGD, normal barium swallow and no improvement with non-pharmacological measures). The case was extensively discussed and there was a consensus to proceed to surgery.
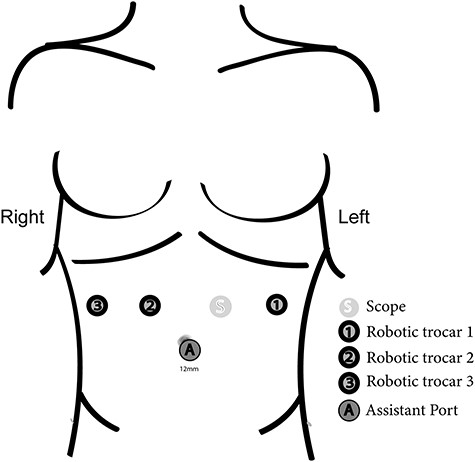
The operation was performed using the Da Vinci Xi (Intuitive Surgical, Sunnyvale, CA). Trocar positioning is shown in Figure 2.
Initially, the left lateral segment of the liver was retracted and the gastro-hepatic ligament was divided to facilitate the identification of the right crus of the diaphragm. The local anatomy made difficult to access the celiac trunk through the gastro-hepatic ligament. The lesser sac was approached opening the gastro-colic ligament, and lifting up the posterior wall of the stomach using the robotic third arm. This maneuver also put in tension the left gastric artery making easier to reach the celiac trunk. All associated lymph nodes and fibrotic tissue that were crossing in front of the origin of the common hepatic and splenic artery were removed (Fig. 3). The dissection continued along the common trunk (Fig. 4). Neural fibers were divided and the origin of the celiac artery was fully exposed free (Fig. 5). Postoperative course was uneventful and the patient was discharged the next day without any dietary restriction. The pain was managed with acetaminophen only after discharge. At 5 months follow up, the patient showed complete resolution of symptoms.
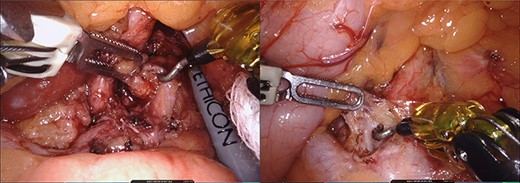
Intraoperative images during lymphanedectomy. Legend: left: lymphadenectomy on the left side of the celiac trunk. Right: lymphadenectomy on the right side of the celiac trunk.
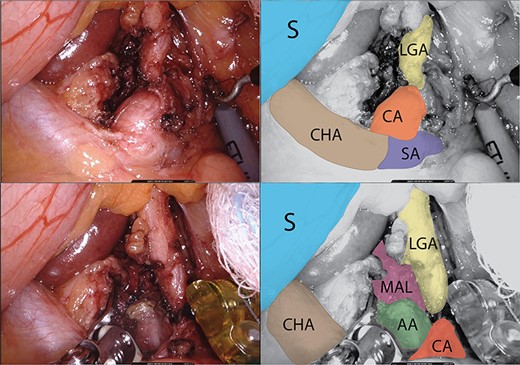
Arterial structures exposure. Legend: upper images: arterial structures before release of the MAL. Lower images: arterial structures during release of the MAL. S: stomach, CHA: common hepatic artery, CA: celiac artery, LGA: left gastric artery and SA: splenic artery.

DISCUSSION
When a low insertion of the MAL or high origin of the celiac artery exists, external compression and narrowing of the celiac artery may occur. In symptomatic patients, other causes of abdominal pain and vomiting should be excluded before confirming the diagnosis of MAL syndrome [5].
Cross-sectional imaging (CT/MR angiography) is usually able to demonstrate the narrowing at the origin of the celiac artery. Doppler ultrasonography is the method of choice when available, as it measures accurately the end-inspiratory and the end-expiratory blood flow velocities in the celiac trunk [6]. Lateral mesenteric angiography with breathing maneuvers is the gold standard for confirming the diagnosis [1, 3].
Laparoscopic decompression of celiac artery, by removing all associated connective and perineural tissue, can offer immediate symptomatic relief and long term maintenance in 85% of patients [4]. Nevertheless, instrument maneuverability is limited and it may lead to a high conversion rate (9–10%) [7].
Robotic surgery has shown promising short-term results [8]. The robotic system can offer a magnified 3D field visualization and instruments with articulated joints [9] allowing increased fluency in motion also within a confined space. These features, combined with the use of the third arm, can also minimize the need for assistant retraction [10]. Tight bands are often adherent to and indistinguishable from the celiac arterial wall, which might be prone to traumatic injury during dissection [7]. The surgeon can perform precise maneuvers with no tremor while creating a safe surgical plane.
This approach is an attractive option for the treatment of MAL syndrome. Treatment success depends upon the appropriate exclusion of other pathologies and an accurate surgical technique. A larger series of robotic cases should be reported to further evaluate the long-term outcomes of this promising technique.
CONFLICT OF INTEREST STATEMENT
Pier C. Giulianotti has a consultant agreement with Covidien Medtronic and Ethicon Endosurgery, and he also has an institutional agreement (University of Illinois at Chicago) for training with Intuitive. The rest of authors don’t have any conflicts of interest.
References
- computed tomography
- epigastric pain
- celiac artery
- constriction, pathologic
- tissue dissection
- ganglia
- pain
- postprandial period
- surgical procedures, operative
- diagnosis
- diagnostic imaging
- surgery specialty
- median arcuate ligament syndrome
- median arcuate ligament
- compression
- median arcuate ligament release



