-
PDF
- Split View
-
Views
-
Cite
Cite
Bardisan Gawrieh, Nabila Salhab, Ammar Omran, Zuheir Alshehabi, Norma Taishori, Wajih Ali, Celiac disease: a rare cause of ‘postoperative’ ileoileal intussusception after surgical reduction of ileocolic intussusception in a toddler, Journal of Surgical Case Reports, Volume 2020, Issue 5, May 2020, rjaa073, https://doi.org/10.1093/jscr/rjaa073
Close - Share Icon Share
Abstract
Intussusception (IS) is defined as invagination of part of the bowel into an adjacent section of the intestines and is the second most common cause of small bowel obstruction in children. Postoperative ileoileal intussusception after surgical reduction is a special type of ileoileal intussusception and is considered idiopathic. This research paper examines the case of a female Syrian toddler who had been diagnosed with ileoileal intussusception after surgical reduction. Diagnosis of celiac disease was later histopathologically confirmed. Celiac disease (CD) may be the underlying cause for special types of intussusception that may be considered idiopathic, and further investigations, such as endoscopy, should be considered.
INTRODUCTION
Idiopathic ileocolic intussusception (IS) is the most common form in children and is typically managed with nonoperative reduction via pneumatic and/or hydrostatic enemas [1–3]. However, recurrence of small bowel intussusception (SBI) is known to be associated with specific pathologies [1, 3]. Awareness of the recurrence of IS and detection of possible pathologies are required, and, thus, early diagnosis is often challenging for pediatricians in a clinical setting [1].

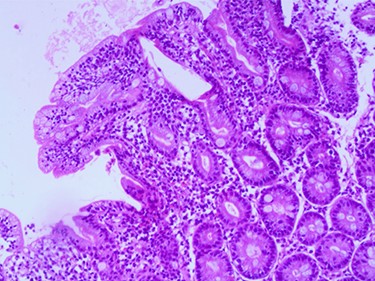
Postoperative ileoileal intussusception after surgical reduction.
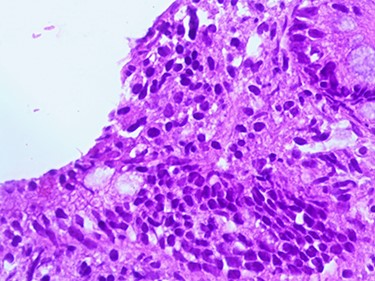
Compatible with Grade B2 on the new grading system for CD classification.
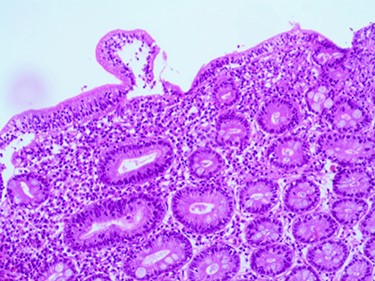
Compatible with Grade B2 on the new grading system for CD classification.
CASE PRESENTATION
A 3.5-year-old Syrian female was admitted to our hospital with complaints of abdominal pain. She had had several episodes of non-bilious, non-bloody vomiting for 36 hours, and her last normal bowel movement was 2 days prior. Although the patient had a history of sickle cell anemia confirmed by electrophoresis from her first year of life, she had not experienced any sickle cell crises and had not needed blood transfusion or hospitalization. She had no history of diarrhea, either. Family history for celiac disease was positive in a second-degree relative. On admission, her vital signs were normal. Blood analysis indicated low hemoglobin (Hgb) concentration of 9.3 g/dl, but other initial laboratory results were normal. Abdominal examination showed tender distended abdomen. Abdominal ultrasonography suggested the presence of intussuscepted bowel in the right iliac fossa with free fluid between the bowels. Hydrostatic reduction (HR) was not successful, so she underwent surgical reduction. Although no lead points were found, there were multiple enlarged mesenteric lymph nodes and edematous ileocecal junction. On the third postoperation day, the patient again developed similar symptoms, and this time ultrasonography revealed IS in the left side of the abdomen. There was no improvement in symptoms for 24 hours, and ultrasonography revealed the same results after an HR attempt. The patient was operated on a second time, and manual ileoileal IS (Fig. 1) reduction and prophylactic appendectomy were performed. The postoperative course was uneventful, and the patient was discharged 3 days later. Three months later, the patient developed abdominal pain, and the diagnosis of IS was confirmed via ultrasonography. This time, IS reduced over 24 hours of observation. As no lead point was found through the later laparotomy, further investigations were conducted. Upper gastrointestinal endoscopy was performed and showed a mosaic pattern of the duodenum mucosa suggestive of CD. On microscopic evaluation, sections reveal advanced atrophy of duodenal villi with occasional intraepithelial lymphocytes (>30/100 IEL). Crypts show moderate hyperplasia; the lamina propria is infiltrated by diffuse mononuclear inflammatory cell infiltrate. Histopathologically, it is compatible with Grade B2 on the new grading system for CD classification (Figs 2–4). The child was then administered with a gluten-free diet. Eight months later, she visited the hospital as outpatient, and examination revealed she was free of any symptoms.
DISCUSSION
IS is a common gastrointestinal emergency in pediatric patients, and it is the most common cause of bowel obstruction in children aged 6–36 months [1–4]. In our case, a 3.5-year-old female was confirmed to have intussusception; as the HR was not successful, she underwent laparotomy, which revealed an edematous ileocecal junction, indicative of spontaneously reduced ileocecal IS. Here we ought to mention that laparoscopy is increasingly the preferred approach for the management of IS reduction and can be performed safely. However, the procedure was not available in the hospital where the study was conducted. In most cases, pediatric ISs are idiopathic in nature and occur at the ileocolic junction. SBI is known to be rare [1–3], and postoperative ileoileal IS after surgical reduction of ileocolic IS in children is a special type of IS and considered idiopathic. Only sporadic reports concerning this unusual type have been reported in the literature. The main clinical characteristics of this type are the following: (i) onset of symptoms is usually within 1 week after the first procedure; (ii) there is reappearance of obstructive symptoms after the intestinal function has been restored and (iii) postoperative ileoileal IS can be easily reduced manually [5]. Likewise, our patient developed abdominal pain on the third postoperation day after the intestinal function had been restored and confirmed to have IS by ultrasonography which considered the diagnostic modality of choice for IS and can also be used to diagnose pathologic lead points when performed by an experienced radiologist [6]. It is difficult to precisely determine the type of IS on ultrasonography even with the presence of few reliable criteria to distinguish between SBI and the more common ileocolic IS [7]. Moreover, in our case the ultrasonography report detected IS but did not determine the type. Although most intestinal ISs at pediatric age are idiopathic, pathological entities could also lead to SBI, such as infections, polyps, lymphomas, malabsorption syndromes, Meckel’s diverticula, duplication cysts, and cystic fibroses [8]. Celiac disease (CD) is an immune-mediated inflammatory disease of the small intestine. It is found in genetically susceptible individuals with exposure to dietary gluten. This disease usually presents with diarrhea, steatorrhea, anemia and weight loss [4, 9]. Although CD may be an underlying cause of IS, associating it with IS before CD diagnosis remains controversial [4, 9, 10]. Our patient, who had a history of sickle cell anemia, had postoperative ileoileal IS, and 3 months after the first intervention, she had spontaneously reduced IS and was later diagnosed with CD. However, owing to an 8-month gluten-free diet, she became free of any symptoms.
CONCLUSION
As most intussusceptions in pediatrics are still classified idiopathic, the reported case demonstrates that what is deemed idiopathic may be associated with an underlying pathological cause. Further investigations, such as endoscopy, may preempt unnecessary surgeries as ISs caused by CD may be transient and resolved spontaneously.
ACKNOWLEDGMENTS
We thank Mr Sami Hanna for providing language help.
CONFLICT OF INTEREST
None declared.



