-
PDF
- Split View
-
Views
-
Cite
Cite
Cassidy Campbell, Edward A Cooper, Philip Kennedy, Emphysematous cholecystitis following routine colonoscopy, Journal of Surgical Case Reports, Volume 2020, Issue 4, April 2020, rjaa091, https://doi.org/10.1093/jscr/rjaa091
Close - Share Icon Share
Abstract
Cholecystitis is a rare sequela of colonoscopy, the relationship between which has not yet been defined. This case study reviews a rural elderly patient who developed right upper quadrant pain following routine colonoscopy. He developed emphysematous cholecystitis, which required laparoscopy with conversion to open via Kocher’s incision and underwent a subtotal cholecystectomy due to the severity of necrosis and inflammation. He had an uncomplicated recovery. Colonoscopy is an important diagnostic procedure, the most common complications of which are haemorrhage and perforation. There are less than 10 cases of associated cholecystitis and no reports of emphysematous cholecystitis. The hypothesized pathogenesis is dehydration and lithogenesis associated with traumatic translocation of organisms, however, no definitive correlation has been determined. Due to the potential health impact, cholecystitis cannot be excluded regarding post-colonoscopy abdominal pain, however, the correlation between procedure and pathology remains unclear.
INTRODUCTION
Cholecystitis is a rare sequela of colonoscopy, the relationship between which has not yet been defined. This case reviews an elderly patient who developed abdominal pain following a routine colonoscopy, which was diagnosed as emphysematous cholecystitis and required surgical intervention. The theorized pathogenesis of post-colonoscopy cholecystitis is dehydration and lithogenesis concurrent with traumatic bacterial translocation associated with colonoscopy, however, no definitive relationship has been determined to date.
CASE REPORT
A 72-year-old man, with a history of type 2 diabetes mellitus, underwent a colonoscopy with standard bowel preparation following a positive faecal occult blood test. He presented to the emergency department 2 days later with increasingly severe right upper quadrant abdominal pain. On questioning, he stated that the abdominal pain had started 3 h following his colonoscopy but he failed to present to hospital earlier as he lived on a rural property more than 2 h away from the nearest medical assistance.
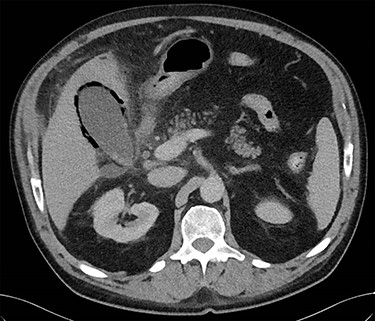
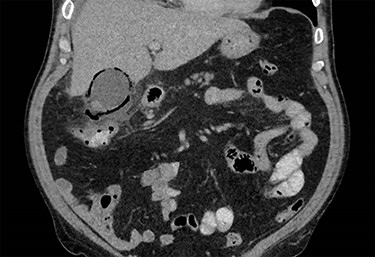
On presentation to the emergency department, the patient was tachycardic and febrile and his serology showed a neutrophilia, elevated CRP and bilirubin with normal hepatic transaminases. On examination, he was focally tender with voluntary guarding in the right upper quadrant. A CT abdomen was performed which identified a distended gallbladder, with adjacent gas locules and fat stranding around the hepatic flexure. The differentials included a contained microperforation at the hepatic flexure or emphysematous cholecystitis. The patient was haemodynamically stable and therefore a period of non-operative treatment was pursued. The patient was commenced on IV ampicillin, metronidazole and gentamicin, strict fluid balance, nil by mouth with regular clinical reviews. On Day 3, the patient had shown minimal clinical improvement and a progress CT was obtained which revealed extensive gas within the gallbladder wall and adjacent-free fluid consistent with emphysematous cholecystitis (Figs 1 and 2).
The patient proceeded to theatre—at laparoscopy, the omentum was wrapped and densely adherent over a firm, thickened and palpable gallbladder. It was unsafe to proceed laparoscopically and the decision was made to convert to a laparotomy. A Kocher’s incision was performed, which revealed a necrotic, gangrenous gallbladder with surrounding seropurulent fluid in the right upper quadrant (Fig. 3). Due to necrosis and oedema of the surrounding anatomy, the cystic duct could not be confidently identified. A subtotal cholecystectomy was completed with an EndoGIA 45 mm articulating stapler used to divide the gallbladder at Hartmann’s pouch. The patient developed a lateral surgical site infection with a superficial wound collection on Day 7, which was drained on the ward and settled with antibiotics prior to discharge.
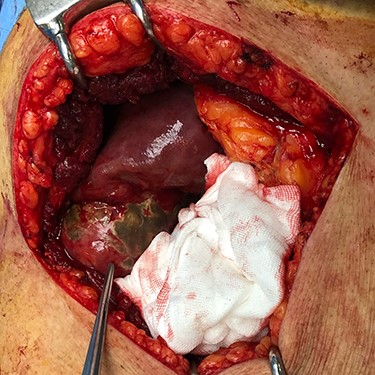
Microbiology of intraoperative swabs grew profuse extended spectrum beta-lactamase-producing Escherichia coli. Histopathology of the specimen reported florid acute on chronic inflammatory changes with extensive mucosal ulceration, oedema and transmural migration of inflammatory cells through the gallbladder wall. This was associated with full thickness necrosis and resulting in perforation at the neck of gallbladder and peritonitis.
DISCUSSION
Colonoscopy is an important diagnostic and therapeutic procedure. While it is well tolerated, it is not without risk. Colonic perforation and haemorrhage are the most common complications with an incidence of ~0.1% [1]. Other documented rare complications include splenic capsular tear, appendicitis, retroperitoneal haemorrhage and an intramural caecal haematoma [2].
In regards to acute cholecystitis following colonoscopy, less than 10 cases have been described in the literature previously [3], with no reports of emphysematous cholecystitis.
Emphysematous cholecystitis is an uncommon variant of cholecystitis. Risk factors include male sex, older age and diabetes mellitus. The most common organisms involved being Clostridia welchii/perfringens and E. coli [4].
The exact mechanism by which acute cholecystitis occurs after colonoscopy is not well established, though it is proposed that the driving factor is the dehydration which develops following bowel preparation and fasting. Dehydration causes the bile to become more lithogenic, with diminished bile flow and bile stasis leading to gallbladder distention [5]. The mechanical manipulation of the colon and the associated bacterial translocation may also play a role in the secondary infection of the gallbladder with enteric pathogens.
Whether cholecystitis following a colonoscopy is due to a chance occurrence of a common condition after a common procedure or whether there is indeed a direct causal relationship between the two remains up for debate. Nevertheless, clinicians should include cholecystitis as a differential diagnosis of acute abdominal pain post colonoscopy.
DISCLOSURE
There are no potential conflicts of interest on the part of any named author.



