-
PDF
- Split View
-
Views
-
Cite
Cite
Holly Calderon, Jennifer Serfin, 13-Hour progression of emphysematous hepatitis as depicted on repeat computerized tomography, Journal of Surgical Case Reports, Volume 2020, Issue 4, April 2020, rjaa089, https://doi.org/10.1093/jscr/rjaa089
Close - Share Icon Share
Abstract
Emphysematous hepatitis is a rare, rapidly progressive and often fatal condition, which occurs predominantly in patients with uncontrolled diabetes mellitus. It results in the replacement of liver parenchyma by a collection of gas. Emphysematous infections of other abdominal and pelvic organs have long been established, but relatively little is known about the equivalent emphysematous infection of the liver with very few examples in the published literature. A review of the literature shows variability regarding timing of presentation and implicated organisms. To date, computerized tomography imaging has been purported to be diagnostic and vital to early management, as it clearly shows the characteristic appearance of air bubbles within the liver parenchyma. We report a case with inconclusive initial radiographic findings.
INTRODUCTION
Emphysematous hepatitis is a rare, rapidly progressive and often fatal condition that results in the replacement of liver parenchyma by gas [1, 2, 3, 4]. This condition was first reported by Blachar et al. [1] in 2002, and to date there are few reports of this condition in the literature [1]. All reviewed cases report fatal outcomes [1–4]. Most reports suggest early imaging by computerized tomography (CT) is diagnostic and will guide clinicians and radiologists to early and aggressive treatment [2–4]. In this case report, we describe a patient with emphysematous hepatitis whose initial CT imaging was inconclusive, and we show the rapid progression of the disease on CT performed 13 h later. We believe this is the first reported case depicting the rapid disease progression from inconclusive to diagnostic on CT imaging.
CASE REPORT
An 80-year-old female with a past medical history of hypertension, diabetes mellitus type 2, chronic kidney disease stage 3, and no known surgical history presented to an acute care hospital emergency department (ED) with an 8-h history of gradual onset upper abdominal pain and nausea. On arrival, the pain was a 9/10 pressure in the right upper quadrant (RUQ) and epigastric regions which the patient described “like the worst gas pain ever.” Vital signs were as follows: temperature 36.4°C, heart rate 69, blood pressure 160/46, respiratory rate 17, SpO2 98%, with a BMI of 50.12 kg/m2. Physical examination was unremarkable except for epigastric and right upper quadrant tenderness without signs of peritonitis. Initial labs: see Table 1.
| Lab . | Value . | Reference . |
|---|---|---|
| CMP | ||
| Blood glucose | 250 | 70–100 mg/dL |
| Alk. phos. | 151 | 44–147 IU/L |
| ALT | 156 | 7–56 U/L |
| AST | 297 | 10–40 U/L |
| Urinalysis | ||
| Glucose | 500 | none |
| Bacteria | 1+ | none |
| Other | ||
| Lactate | 3.2 | 0.5–2.0 mmol/L |
| Lipase | 7326 | 22–51 U/L |
| Lab . | Value . | Reference . |
|---|---|---|
| CMP | ||
| Blood glucose | 250 | 70–100 mg/dL |
| Alk. phos. | 151 | 44–147 IU/L |
| ALT | 156 | 7–56 U/L |
| AST | 297 | 10–40 U/L |
| Urinalysis | ||
| Glucose | 500 | none |
| Bacteria | 1+ | none |
| Other | ||
| Lactate | 3.2 | 0.5–2.0 mmol/L |
| Lipase | 7326 | 22–51 U/L |
| Lab . | Value . | Reference . |
|---|---|---|
| CMP | ||
| Blood glucose | 250 | 70–100 mg/dL |
| Alk. phos. | 151 | 44–147 IU/L |
| ALT | 156 | 7–56 U/L |
| AST | 297 | 10–40 U/L |
| Urinalysis | ||
| Glucose | 500 | none |
| Bacteria | 1+ | none |
| Other | ||
| Lactate | 3.2 | 0.5–2.0 mmol/L |
| Lipase | 7326 | 22–51 U/L |
| Lab . | Value . | Reference . |
|---|---|---|
| CMP | ||
| Blood glucose | 250 | 70–100 mg/dL |
| Alk. phos. | 151 | 44–147 IU/L |
| ALT | 156 | 7–56 U/L |
| AST | 297 | 10–40 U/L |
| Urinalysis | ||
| Glucose | 500 | none |
| Bacteria | 1+ | none |
| Other | ||
| Lactate | 3.2 | 0.5–2.0 mmol/L |
| Lipase | 7326 | 22–51 U/L |
CT of the abdomen and pelvis with IV contrast was performed within 2 h of presentation. The scan showed “indeterminate, scattered ill-defined hypo-enhancing lesions in the liver with no acute etiology identified to explain the patient’s abdominal pain” (Figs 1, 3, 5). The remainder of the CT was unremarkable. Ultrasound (US) of the abdomen was negative. Because the CT and US did not identify an etiology for the patient’s abdominal pain, the working diagnosis at that time was an intestinal obstructive process.
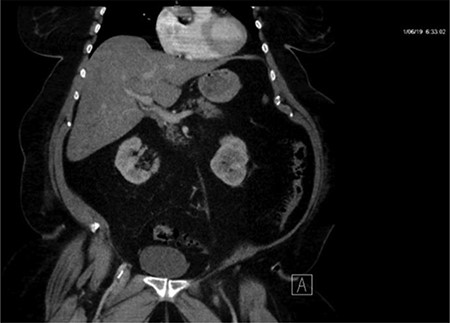
CT with IV contrast taken at 0633 which shows ill defined, hypo-enhanced lesions of the liver.
| Lab . | Value . | Reference (Unit) . |
|---|---|---|
| ABG | ||
| pH | 7.21 | 7.35–7.45 |
| pCO2 | 39.0 | 32–45 (mmHg) |
| Bicarb | 15.6 | 18–23 (mmol/L) |
| Urinalysis | ||
| Glucose | 1000 | None (mg/dL) |
| Blood | 250 | None (μL) |
| Protein | 30 | None (mg/dL) |
| Other | ||
| Lactate | 10.9 | 0.5–2.0 mmol/L |
| POCT glucose | 182 | 70–99 mg/dL |
| Lab . | Value . | Reference (Unit) . |
|---|---|---|
| ABG | ||
| pH | 7.21 | 7.35–7.45 |
| pCO2 | 39.0 | 32–45 (mmHg) |
| Bicarb | 15.6 | 18–23 (mmol/L) |
| Urinalysis | ||
| Glucose | 1000 | None (mg/dL) |
| Blood | 250 | None (μL) |
| Protein | 30 | None (mg/dL) |
| Other | ||
| Lactate | 10.9 | 0.5–2.0 mmol/L |
| POCT glucose | 182 | 70–99 mg/dL |
| Lab . | Value . | Reference (Unit) . |
|---|---|---|
| ABG | ||
| pH | 7.21 | 7.35–7.45 |
| pCO2 | 39.0 | 32–45 (mmHg) |
| Bicarb | 15.6 | 18–23 (mmol/L) |
| Urinalysis | ||
| Glucose | 1000 | None (mg/dL) |
| Blood | 250 | None (μL) |
| Protein | 30 | None (mg/dL) |
| Other | ||
| Lactate | 10.9 | 0.5–2.0 mmol/L |
| POCT glucose | 182 | 70–99 mg/dL |
| Lab . | Value . | Reference (Unit) . |
|---|---|---|
| ABG | ||
| pH | 7.21 | 7.35–7.45 |
| pCO2 | 39.0 | 32–45 (mmHg) |
| Bicarb | 15.6 | 18–23 (mmol/L) |
| Urinalysis | ||
| Glucose | 1000 | None (mg/dL) |
| Blood | 250 | None (μL) |
| Protein | 30 | None (mg/dL) |
| Other | ||
| Lactate | 10.9 | 0.5–2.0 mmol/L |
| POCT glucose | 182 | 70–99 mg/dL |
On re-evaluation, the patient was awake, alert, oriented and hemodynamically stable. Repeat blood work demonstrated an increase in lactate level from 3.2 to 6.8 mmol/L within 5 h, despite aggressive fluid resuscitation (see Table 2). She was subsequently transferred from the ED to a regional medical center with ICU capabilities. On arrival, her condition had deteriorated significantly. She required intubation shortly after admission to ICU.
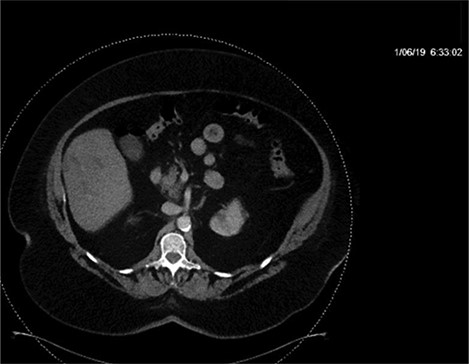
Repeat CT demonstrated a large amount of air within the liver parenchyma (Figs 2, 4, 6). Unfortunately, shortly after the repeat CT, the patient progressed to septic shock with cardiovascular collapse and was not able to be resuscitated with full advanced cardiac life support (ACLS) protocol. She expired within 16 h of initial presentation and within 24 h of symptom onset. Final blood culture results were positive for Clostridium perfringens.
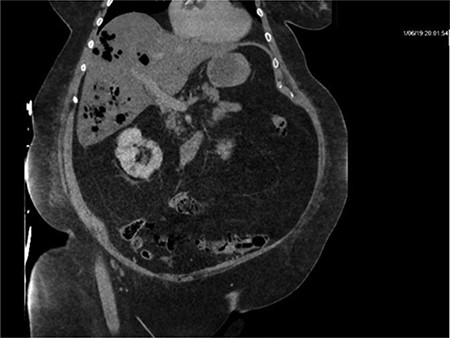
Repeat imaging taken 13.5 h later which depicts many air bubbles in the liver parenchyma.
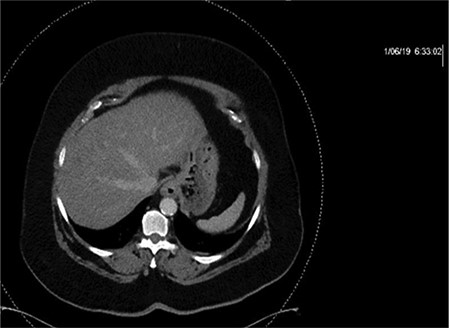
CT with IV contrast taken at 0633 which shows ill defined, hypo-enhanced lesions of the liver.

Repeat imaging taken 13.5 h later which depicts many air bubbles in the liver parenchyma.
CT with IV contrast taken at 0633 which shows ill defined, hypo-enhanced lesions of the liver.

Repeat imaging taken 13.5 h later which depicts many air bubbles in the liver parenchyma.
DISCUSSION
Emphysematous hepatitis is a condition with insidious onset, rapid progression and fatal outcomes in all reviewed cases [1–4]. Due to the limited literature describing this condition, it has been compared to emphysematous diseases of other organs. It has a preponderance in those with poorly controlled diabetes [5]. Patient presentation usually starts with abdominal pain as an initial complaint, with fever and altered mental status as later manifestations [5]. It is definitively diagnosed by the presence of gas within the parenchyma of the liver as seen on CT imaging.
Other emphysematous infections with nearly identical pathophysiology have occurred in the stomach, gallbladder, pancreas and throughout the genitourinary system [5]. All, except for emphysematous uterus or vaginitis, carry a high mortality rate ranging from 15 to 80%, and involve an insidious manifestation, rapid progression to sepsis and gas formation seen on imaging [5].
The pathophysiology involves the fermentation of glucose by the causative bacteria, which produces a gaseous mixture of 60% nitrogen, 15% hydrogen, 5% carbon dioxide and 5% oxygen [2]. Emphysematous infections are common in those with diabetes due to the increased blood glucose facilitating fermentation [2]. Organisms implicated in the literature for cases of emphysematous hepatitis are.
Streptococcus mutans, Enterococcus faecalis, Klebsiella pneumoniae, Enterobacter cloacae and C. perfringens [1, 3, 4].
Current literature suggests CT imaging as vital to early diagnosis of emphysematous hepatitis since it clearly depicts air in tissue [2–4]. As described, this was not true for the present case. The patient in the current report presented earlier than others in the reviewed literature after only 8 h of symptoms. The initial CT was done within 2 h of presentation and did not depict the air bubbles that would appear on repeat imaging 13 h later. This is the first case of all reviewed with inconclusive CT imaging associated with the acute presentation of this diagnosis. This suggests early presentation may not improve outcomes since, as seen here, the patient presented early and had an inconclusive initial CT, with the characteristic emphysematous bubbles only seen on repeat CT performed immediately before expiration.
The proposed treatments for emphysematous infections of the abdomen and pelvis include broad spectrum antibiotics, surgical drainage or removal of any obstruction, as well as correction of hyperglycemia, acid-base imbalance and electrolyte abnormalities [5]. However, treatment has been unsuccessful to date. Lab results appear to change almost as rapidly as the imaging studies with aspartate aminotransferase (AST) and alanine aminotransferase (ALT) values increasing from the hundreds to the thousands within hours [3, 4]. If imaging and lab results change too quickly to be of assistance in treating this fulminant and rapidly fatal condition, then pre-emptive and empiric antibiotic treatment is suggested.
CONCLUSION
Emphysematous hepatitis is a condition in which liver parenchyma is replaced with a collection of gas produced by fermenting organisms and is associated with insidious manifestation, rapid progression and grave prognosis [1–4]. We believe this is the first reported case depicting the rapid disease progression from inconclusive to diagnostic on CT imaging. This case demonstrates that CT imaging is not always conclusive. We suggest that emphysematous hepatitis be included in the differential diagnosis in patients presenting with otherwise unexplained right upper quadrant abdominal pain, and that broad-spectrum antibiotics and aggressive resuscitation should be initiated empirically. Further evaluation of treatment options is necessary to improve the outcome of this condition.
ACKNOWLEDGEMENTS
The authors have no financial disclosures.
CONFLICTS OF INTEREST
The authors declare that there is no conflict of interest regarding the publication of this article.
FUNDING
Funding was provided by Good Samaritan Regional Medical Center, Corvallis, OR - Graduate Medical Education and the Department of Surgery.



