-
PDF
- Split View
-
Views
-
Cite
Cite
Timothy M Guenther, Joshua D Gustafson, Curtis J Wozniak, Scott A Zakaluzny, Garth H Utter, Penetrating thoracic injury from a bean bag round complicated by development of post-operative empyema, Journal of Surgical Case Reports, Volume 2020, Issue 4, April 2020, rjaa078, https://doi.org/10.1093/jscr/rjaa078
Close - Share Icon Share
Abstract
Bean bag guns were developed as a nonlethal means for law enforcement personnel to subdue individuals. The large surface area and lower velocities of the bean bag round theoretically result in transfer of most of the energy to the skin/subcutaneous tissue and minimize the likelihood of dermal penetration, thereby ‘stunning’ intended victims without causing injury to deeper structures. However, this technology has been associated with significant intra-abdominal and intrathoracic injuries, skin penetration and death. We present a 59-year-old man who sustained a penetrating thoracic injury from a bean bag gun. Although the bean bag was successfully removed, the patient developed a postoperative empyema requiring operative management. We discuss the unique aspects of thoracic trauma from bean bag ballistics as well as considerations in management of patients with this uncommon mechanism of injury.
INTRODUCTION
Bean bag guns were first developed in the 1970s as a nonlethal means for law enforcement personnel to subdue individuals without resorting to lethal force [1]. A bean bag round weighing approximately 40–50 g is accelerated at a velocity of 230–300 feet/second, thereby ‘stunning’ the intended victim [2]. The large surface area of a bean bag round is thought to disseminate the kinetic energy of the ballistic upon impact and theoretically prevent penetration through the dermis [3]. However, cases involving serious intra-abdominal/intrathoracic injury, skin penetration and death from these projectiles have been reported [4]. We report a 59-year-old man who sustained a penetrating thoracic injury from a bean bag round. Although the projectile was removed, the patient’s course was complicated by the development of a post-operative empyema requiring surgical drainage and decortication.

Initial anteroposterior and lateral chest X-rays of the patient, consistent with intrathoracic penetration of the bean bag foreign body.
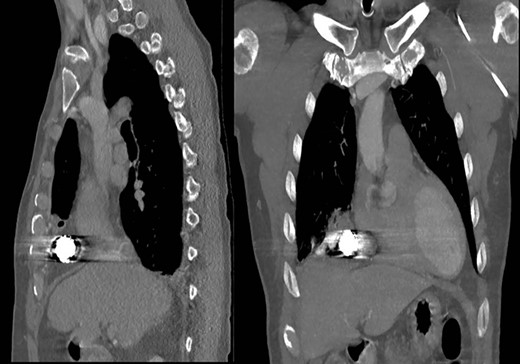
Representative coronal and sagittal images of the patient’s initial chest CT scan confirming the intrathoracic location of the foreign body with associated scatter due to its metallic contents.
CASE REPORT
A 59-year-old man was transferred acutely from another hospital for evaluation of a penetrating thoracic injury. The patient reportedly had been shot twice with a bean bag gun and sustained injuries to the right chest and flank during an altercation with police officers. The patient was breathing comfortably and normotensive, and his GCS was 15. He had a history of unprovoked pulmonary embolism and was taking apixaban. There was a 2-cm circular wound through the skin just superior to the right nipple and a 5-cm area of ecchymotic but intact skin over the right flank. A chest X-ray showed a 2-cm object with metallic density overlying the right thoracic cavity (Fig. 1). A chest CT showed the object in close proximity to the right atrium, right internal mammary artery and right middle lobe (Fig. 2). Additionally, a small amount of effusion consistent with hemothorax was present, for which a chest tube was placed. The patient was admitted for chest tube management and pain control, on the assumption that the metallic foreign body did not warrant operative removal.

Operative image of the removed intrathoracic bean bag with intact Kevlar coating.
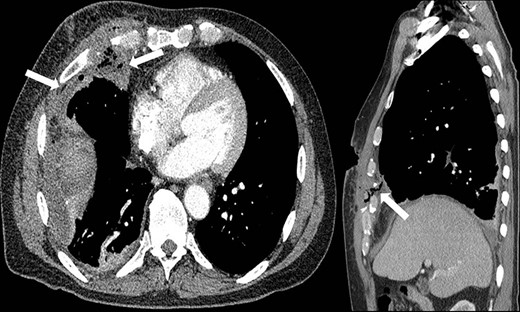
Representative axial and sagittal images from the patient’s CT scan on Day 7 after initial operative intervention. The white arrows on both images show subcutaneous and intrathoracic air, concerning for an empyema.
Subsequent review of bean bag projectiles and discussion with the law enforcement officers monitoring the patient revealed that the bean bag projectile included nonmetal components. Out of concern for infection risk, the surgical team performed video-assisted thoracoscopic surgery (VATS) on hospital Day 3 whereby the projectile was successfully removed (Fig. 3). Upon intra-operative inspection, the right middle lobe was contused but not actively bleeding, so no further intervention was performed, and a new chest tube was placed. On post-operative day (POD) 3, the chest tube was removed; however, on POD 6 purulent drainage was observed from the previous bean bag entry wound, and laboratory evaluation revealed a leukocytosis to 21.0 K/mm3. The clinicians irrigated the wound at the bedside and initiated antibiotics treatment. Due to persistent leukocytosis and drainage of purulent fluid from the wound, the clinicians obtained a CT scan on POD 7, which showed a complex right pleural effusion that communicated with a small pocket of fluid in the chest wall, concerning for an empyema (Fig. 4). The following day, the surgeons performed VATS decortication, removing a significant amount of purulent pleural fluid and fibrinous exudate and placing two chest tubes. Culture of the pleural fluid grew Staphylococcus aureus. By POD 11/3, the patient had a persistent right-sided effusion, which the team treated with intrapleural tPA/Dornase infused via previously placed chest tubes. By POD 20/12, the patient’s leukocytosis and right-sided effusion had resolved, and both chest tubes were removed. He was discharged the subsequent day and has not returned to our facility since then.
DISCUSSION
The thorax is the body region most commonly affected among patients with bean bag gun-related trauma that seeks medical care [4]. This is likely related to the size of the thorax and its central location where law enforcement officers are often trained to aim when delivering lethal force [5]. The relatively decreased volume of soft tissue over the thorax may make it more susceptible to increased damage compared to other parts of the body because less energy is absorbed by the dermis and subcutaneous tissue [6]. Non-penetrating thoracic injuries from bean bag rounds most commonly lead to skin ecchymosis, broken ribs and pulmonary/cardiac contusions with deeper transfer of energy [7]. Penetrating thoracic injuries from bean bag ballistics are much less common and can be associated with pulmonary/cardiac contusions, lacerations and death [2, 8].
Although less lethal than conventional firearms, bean bag gun injuries can result in serious harm, and it is important for surgeons to recognize the unique injury patterns and characteristics of these projectiles [9]. Surgeons should strongly consider operative removal of retained bean bags or their fragments. Studies of conventional metallic bullets have shown that infection and complication rates remain low in instances in which embedded bullets are not removed; thus routine removal is not recommended [10]. However, bean bags—though they may appear only metallic on radiographs—are composed of numerous metallic pellets, possibly with cotton packing, covered with a layer of Kevlar or other fabric. Thus, the large, complex surface of these projectiles likely entrains bacteria, other foreign bodies (e.g. hair or clothing particles) and devitalized tissue in the wound, substantially increasing the risk of infection, as occurred in this patient. Additionally, surgeons should exercise care when handling bean bags to minimize the risk of spillage of the metallic pellets into the wound, which can lead to increased operative time and post-operative complications [4].
In conclusion, penetrating thoracic trauma from bean bag ballistics represents a rare complication of their use. Clinicians should be aware of the unique characteristics of such injuries and specifically consider prompt surgical removal of retained bean bags to minimize the risk of infection.
CONFLICT OF INTEREST STATEMENT
The views expressed in this material are those of the authors and do not reflect the official policy or opinion of the U.S. Government, the Department of Defense, or the Department of the Air Force.
ACKNOWLEDGEMENTS
None.
The work was not presented at any scientific meeting.



