-
PDF
- Split View
-
Views
-
Cite
Cite
Yukio Yoshioka, Yasutaka Hayashido, Yoku Ito, Shigeaki Toratani, Tetsuji Okamoto, Reconstruction of an upper lip and intraoral defect following resection of an upper lip melanoma using a lower lip musculomucosal flap combined with a tongue flap, Journal of Surgical Case Reports, Volume 2020, Issue 4, April 2020, rjaa072, https://doi.org/10.1093/jscr/rjaa072
Close - Share Icon Share
Abstract
Restoring the cosmetic and functional aspects of the lip after tumor resection is challenging. We report a case of reconstruction for a defect due to resection of a melanoma using a lower lip musculomucosal flap combined with a tongue flap. A 20-year-old man was referred to our hospital and diagnosed with malignant melanoma with metastatic right submaxillary lymph nodes. We excised the tumor with neck dissection. We excised not only the right upper lip mucosa but also the gum, including some orbicularis oris muscle and alveolar bone from the right canine tooth to the left central incisor tooth. The defect was simultaneously reconstructed using both, a lower lip musculomucosal flap and a tongue flap. Revisional operation to remove contraction of a postoperative scar and the right vermillion border collection was performed at 3 months after the initial operation. There had been no functional and cosmetic trouble of the upper lip.
INTRODUCTION
Reconstruction of a lip defect following resection of a malignant tumor requires restoration of both the function and the aesthetics of the lip. Function implies sensation and movement of the reconstructed oral sphincter; aesthetics demands that the color and texture match that of the lip. Generally, a defect less than a third of the lip can be closed primarily. Total lip reconstruction requires not only free flaps and/or distant pedicle flaps but also local flaps such as Bernard–von Burrow–Webster flaps, Gillies fan flaps, Fujimori gate flaps and modified von Brun flaps [1]. In cases where lip defects are relatively large (between 30 and 80%), local rotational flaps such as Abbé and Estlander flaps are often used [1, 3]. Defects at the center of the lip often require Abbé flaps; in cases of oral commissures, Estlander flaps are used. In addition to these two excellent methods, mucosal advancement flap is also a well-established method for lip reconstruction. Manafi et al. reported a successful cross-lip technique to restore the vermillion border using a lip musculomucosal flap [2]. Such a lip musculomucosal flap is often used for reconstruction of the vermillion border, and a tongue musculomucosal flap is used to fill relatively larger intraoral defects [3]. We report a reconstruction of an upper lip and perioral defect following melanoma resection using a musculomucosal flap with a tongue flap compensating for both blood supply and defect volume.
CASE REPORT
A 20-year-old male patient was referred to our hospital with a small black-colored polyp on the upper lip. On clinical examination, a small polyp measuring 10 × 8 mm in size at the right side of the upper lip mucosa with a brown–black patch expanding from gingivolabial sulcus to the attached gum of incisor tooth was observed (Fig. 1). He was clinically diagnosed with a mucosal malignant melanoma with a metastatic right submaxillary lymph node (Fig. 2). The brown–black patch was melanoma in situ. The polyp was found to be a malignant melanoma following a biopsy. Tumor resection with radical neck dissection was performed 5 days after the biopsy. The tumor excision site was planned, involving some orbicularis oris muscle, including oral mucosa, gingiva and alveolar bone extending from the right canine tooth to the left central incisor tooth (Fig. 3). The defect in the red lip was reconstructed using a musculomucosal flap from the lower lip; simultaneously, the perioral defect was reconstructed using a tongue flap. Initially, the intraoral defect was filled using a tongue flap to the greatest extent possible (Fig. 4). A 10-mm width musculomucosal flap including the right inferior labial artery, in which blood flow had been detected using Doppler ultrasound after right side neck dissection, was designed at the lip mucosa, reaching the left side beyond the center of the lip (Fig. 5). Both the right vermillion border and the shortage of intraoral reconstruction by the tongue flap were repaired using a lip musculomucosal flap (Fig. 6). Both flaps healed well without any congestion or necrosis. They were separated at 2 weeks after primary surgery under deep sedation. The patient could eat and speak without trouble. Nevertheless, cupid’s bow was conspicuous for the gap and the postoperative scar contracted after 3 months. Therefore, correction of the cupid’s bow using Z-plasty of the white lip and reduction of the tongue flap was performed. The secondary operation to correct the misalignment of cupid’s bow and to remove the contraction was successful (Fig. 7).

Intraoral photograph of the initial examination. A small mass measured 10 × 8 mm in size at the right side of the upper lip mucosa with a brown–black patch expanding from gingivolabial sulcus to the attached gum of incisive tooth was observed.
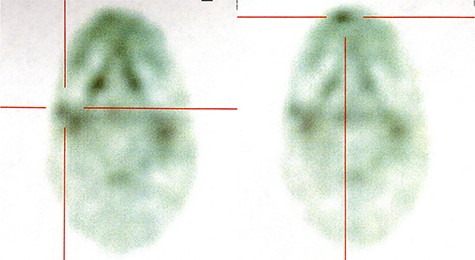
Positron emission tomography/CT finding. 18F-FDG accumulated at both right submaxillary lymph node (left) and right upper lip (right).

Operative finding. The tumor was excised with some orbicularis oris muscle including the oral mucosa, gingiva and alveolar bone from the right canine tooth to the left incisor.
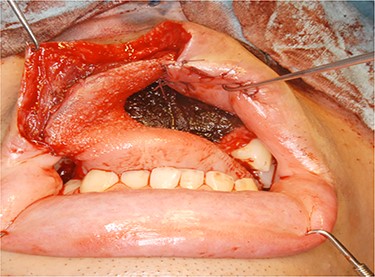
Operative finding. Intraoral defect was filled with a tongue flap.
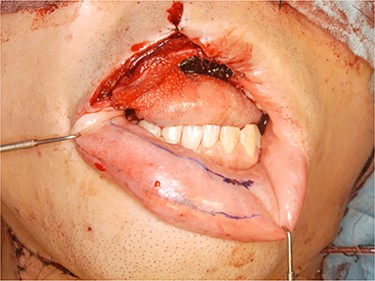
Operative finding. Lower lip musculomucosal flap of 10-mm width was designed at lip mucosa reaching the left side beyond the center of the lip.

Operative finding. Vermillion border was restored using a lower lip musculomucosal flap.
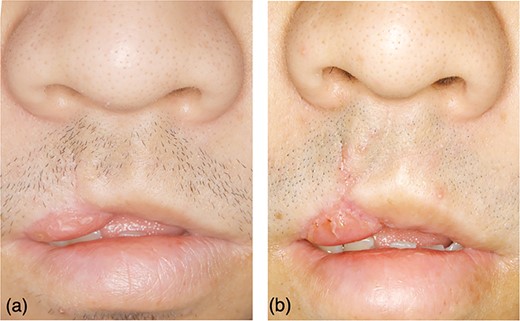
The secondary operation to correct the misalignment of cupid’s bow and remove the contraction. (a) Three months after primary surgery, cupid’s bow was conspicuous for a gap, and the tongue flap became contracted. (b) Collection of cupid’s bow using Z-plasty of white lip and reduction of tongue flap.
DISCUSSION
In the present case, the defect left by extended resection of melanoma was relatively large. It included about a half of the upper red lip without the white lip and oral mucosa and alveolar bone corresponding to four upper front teeth. According to the algorithm for lip reconstruction [4], an Abbé flap might be suitable for the reconstructive technique. However, this was not chosen because his white lip had not been resected; furthermore, the intraoral defect might have been too large to be restored using an Abbé flap. An oral musculomucosal local flap would be more suitable to restore the color and texture of oral mucosa. Pribaz et al. reported a facial artery musculomucosal (FAMM) flap in 1992 [5]. This is an axial flap that has adequate blood supply from the facial artery and consists of mucosa, submucosa, some buccinator muscle and orbicularis oris muscle, facial artery and submucosal venous plexus [6, 7]. Many clinicians found that this flap is versatile enough to not only restore the defect of lip, floor of mouth, alveolar bone and oral vestibule, but also to repair an oronasal fistula and nasal septal perforation [6–9]. Considering only the site and volume of defect in the present case, reconstruction by the superiorly based flow FAMM might be more appropriate than any other local flap. However, neck dissection without preserving a facial artery had to be performed in the present case because melanoma had metastasized to submaxillary gland lymph nodes. Therefore, FAMM flap was not used because it might have become necrotic. According to Ferrari et al., neck dissection preserving the facial artery to design FAMM flaps in cases without regional metastasis does not alter the rate of regional recurrences [10]. In the present case, neck dissection preserving the facial artery could not be performed because the risk of submaxillary lymph node metastasis would have been substantial. An inferior labial flap, fed by the labial artery branched from facial artery, was used instead of a FAMM flap. An ipsilateral flap alone might have become necrotic along with the FAMM flap. The right lip musculomucosal flap extended to the left/opposite side, so that it would have blood supply from anastomoses between both sides of the artery. A tongue musculomucosal flap is a conventional local flap, with abundant blood supply available for large defects. It had been used safely for congenital clefts and defects left by tumor resection. The lip musculomucosal flap combined with tongue flap produces good outcome in cases of lip and intraoral defects caused due to tumor resection and neck dissection.
ACKNOWLEDGMENTS
Anatomical advices and comments provided by Prof. Ryuji Terayama (Department of Maxillofacial Anatomy and Neuroscience, Hiroshima University) were of great help in this study. We would like to thank Editage (www.editage.jp) for English language editing.
CONFLICT OF INTEREST
None declared.



