-
PDF
- Split View
-
Views
-
Cite
Cite
Abdullah A Alturki, Sarah A Aldeghaither, Ali A Alhandi, Severe heterotopic ossification post total knee arthroplasty in a patient with rheumatoid arthritis: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjz390, https://doi.org/10.1093/jscr/rjz390
Close - Share Icon Share
Abstract
Stiffness following total knee arthroplasty (TKA) can be a devastating complication to the patient by limiting his function. Various causes have been reported in the literature, including heterotopic ossification (HO). HO is one of the rarely reported complication of TKA characterized by deposition of bone cells in non-skeletal tissue. This is a case of 32-year-old female known to have rheumatoid arthritis with history of TKA 4-years-ago complaining of right knee pain and restricted range of motion. She was later found to have HO and was treated with a revision TKA. In conclusion, the incidence and outcome of HO following total knee replacement in patients with RA remains underexplored topic in the literature.
INTRODUCTION
Stiffness following total knee arthroplasty (TKA) can be a devastating complication to the patient by limiting his function. Various causes of knee stiffness following TKA have been reported in the literature, including arthrofibrosis, oversizing of components, incorrect gap balancing and heterotopic ossification (HO). HO occurs when primitive mesenchymal cells in the surrounding soft tissues are transformed into osteoblastic tissue. The incidence rate of HO following TKA is a point of contention in the literature with reported ranges between 4 and 40%. However, it rarely has an impact on clinical outcome [1].
This case reports an unusual presentation of rheumatoid arthritis patient who had undergone primary TKA, which was complicated by severe HO resulted in zero range of motion.
CASE PRESENTATION
A 32-year-old female known case of rheumatoid arthritis affecting both knees presented to our clinic complaining of severe right knee stiffness post TKA 4-years-ago done in an outside facility (Figs. 1 and 2). She lives in a rural community and was on hydroxychloroquine, but her disease was active as she was not compliant to her medication. On physical examinations, the right knee was larger in size compared to the left knee without joint effusion. Range of motion was zero on flexion, −10° in extension. Standing knee X-ray showed HO around the prosthesis (Fig. 2). Computed tomography (CT) demonstrated extensive HO with implants fixed in place (Fig. 3). Revision surgery and replacement of the prostheses was considered to restore function.

Preoperative X-ray of the knee before the primary operation showing severe osteoarthritis changes.
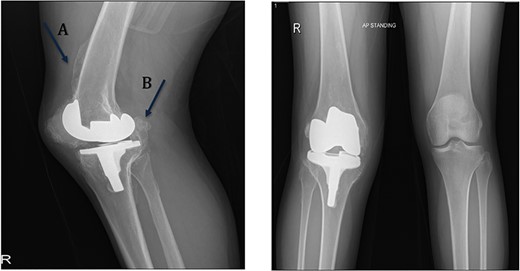
Preoperative standing X-ray showing heterotopic ossification around the prosthesis with preserved knee joint. (A) Heterotopic bone extending proximally on the anterior surface of the femur. (B) Posterior heterotopic bone fusing the knee joint. Careful removal with osteotomes and bone curettes was necessary to remove the old implants.
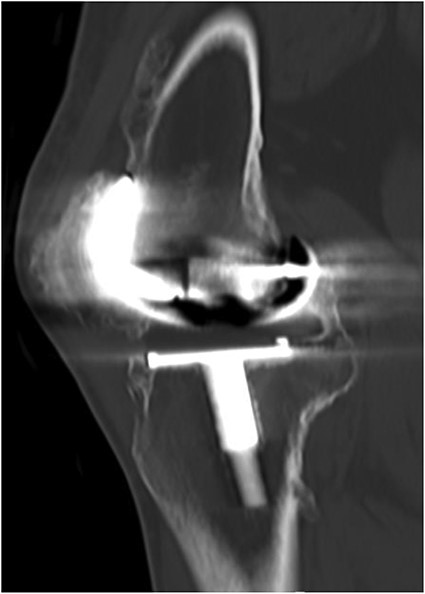
CT demonstrated extensive heterotopic ossification involving the popliteal fossa, the anterior surface of the patella and at the distal third of anterior femur extending to the level of the knee-replacement prosthesis. There was no evidence of implant looseness or alignment deformity and there was no evidence of progressive ossification.
Procedure
The old medial parapatellar approach was utilized. The medial and lateral gutters were completely released up to the posteromedial corner. When the knee was too stiff to be mobilized further, the patellar tendon was found to be severely contracted and shortened with patella baja deformity. A tibial tubercle osteotomy was needed for adequate exposure. Osteotomy fragment measured 6 cm with 1.5 cm thickness, after which we became able to flex the knee. The components were completely engulfed by capsular heterotopic bone (Fig. 2). Using osteotomes and burrs, the tibial and the femoral components were slowly visualized. Both components were found to be well fixed. Carful removal of the posterior heterotopic bone was done with a bone curette, which finally allowed for component removal. Intraoperative culture samples were taken as routine measure for revision surgeries. RT-Plus modular rotating hinge knee system (Smith & Nephew, Memphis, TN, USA) was used. The procedure was started with reaming the tibia up to size 12 mm. It was sized to be size four. Proximal drilling and rasping were done, and posterior offset stem was used.
After that, reaming of the femur was carried out reaching size 14 mm, giving a good fixation. Distal resection was done followed by posterior resection and box preparation. Afterward, the implants were cemented into place. The knee was in full extension with excellent stability. Attention was then taken to realign the patella. Osteotomy fragment was moved proximally 1 cm and fixed with 3.5 cortical screws achieving bicortical fixation. Bone graft was used for the remaining osteotomy site.
On the table, range of motion was 0–90°. Intraoperative image intensifier was used and demonstrated excellent position of the implant and the osteotomy site (Fig. 4).
Follow up
Postoperatively, she could flex her knee up to 90° in bed. Cultures were negative and upon discharge, she was referred to rheumatology department for review. She was started on disease-modifying antirheumatic drugs DMARDs. She was also put on indomethacin for 6 weeks for HO prophylaxis. In the immediate post-operative period, she was able to maintain 90° of flexion and full extension using continuous passive motion machine only.
The patient lost some of her range of motion (ROM) in the post-operative period even with extensive physiotherapy. On her 4-month follow up appointment; ROM was 10–80°, which she sustained afterward. Plain radiographs continued to show no new HO formation at 4 months (Fig. 5).

Intraoperative image intensifier demonstrated position of the implant, screw and the osteotomy site.
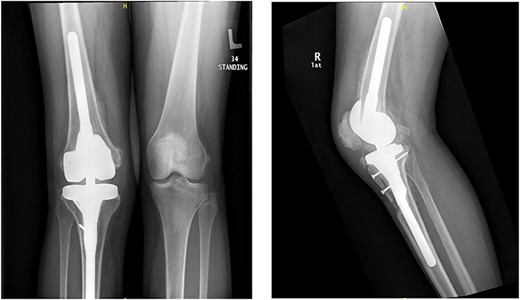
Knee X-rays at 4 months visit continued to show no new HO formation, and continuation of healing of the osteotomy.
DISCUSSION
TKA in RA patients has shown excellent results in the literature when compared to osteoarthritis patients [2–8]. The pathology of RA affecting the knee joint makes TKA an attractive option for patients failing medical therapy. One Study by Kumagi et al. even suggested an effect on disease activity post TKA. Their team noted a decrease in disease activity post TKA, which was attributed to effect of the synovectomy during surgery [7]. With all the possible complications post TKA, HO remains a largely underexplored topic compared to HO post total hip replacement [9]. Prophylaxis against HO post joint replacement remains the main discussion point [1]. Nonsteroidal anti-inflammatory drugs (NSAIDs) and radiotherapy seem to be the only feasible options for prophylaxis pre and post HO development. Multiple randomized controlled trials and literature reviews addressed the difference between the two modalities with varying degrees of success in the THA related literature. Timing, duration of treatment and dosages are three discussion points with no clear consensus [1]. Combination therapy was also studied in a two retrospective studies, but no randomized controlled trials were noted. The decision was made to treat this patient with Indomethacin for prophylaxis against HO for its ease of use.
Treatment of HO post TKA necessitates a surgical intervention when it interferes with function. NSAIDS and radiotherapy have no role post development and extensive physiotherapy has no published research supporting its efficacy. A revision TKA was needed for this patient due to the sever HO development. Intraoperatively, a complete release of the medial and lateral gutters resulted in unstable knee joint, which necessitated a hinge-knee prosthesis. The effect of tibial tubercle osteotomy on post-operative rehabilitation was also considered, but due to the severely shortened extensor mechanism, it was needed for exposure. A recent case series by Eid et al. even went as far as to recommend the osteotomy for all RA patients. We considered the possible effect of indomethacin on healing post osteotomy, but the decision was made to move forward with the treatment as options were limited. The loss of ROM noted is currently attributed to patient lack of adherence to her physiotherapy regimen and the general weakness of her thigh muscles, as there is no radiographic evidence that would prevent her from gaining more ROM.
A review of a large sample size specifying the incidence and outcomes of HO post TKA in RA patients is highly recommended at this stage, due to the complexity of the disease process and its inevitable effects on HO formation. Furthermore, no clear consensus was found in the literature regarding the possible etiology and risks for such a presentation, and due to the rarity of the presentation it would be difficult to properly study.
Conflict of interest statement
The authors declare no conflicts of interest.
Acknowledgments
This case is supported by King Abdullah International Medical Research Center, Riyadh, KSA but through no dedicated source of funding.
Author’s contribution
A.A. Alturki was the patient’s orthopedic surgeon, interpreted the imaging findings and contributed to manuscript drafting.
S.A.A. reviewed the literature and contributed to manuscript drafting.
S.A.A. reviewed the literature and contributed to manuscript drafting.
A.A. Alhandi reviewed the literature and drafted the manuscript. All authors issued approval for the final version.



