-
PDF
- Split View
-
Views
-
Cite
Cite
Keith George, Shane Burke, Sandra Park, Luis Suarez, Ron Riesenburger, Presentation and management of IVC and iliac vein encroachment by lumbar pedicle screws: a case-report, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjaa040, https://doi.org/10.1093/jscr/rjaa040
Close - Share Icon Share
Abstract
Pedicle screws are commonly used in spinal surgeries and are relatively safe, with venous complications occurring rarely. We report a patient with imaging following a L4–5 fusion that showed indentation of the inferior vena cava and right common iliac vein by the right L4 and L5 pedicle screws. She underwent revision surgery in which the hardware was removed and no bleeding was observed. Intraoperative venogram confirmed vascular integrity and absence of indentation on the venous structures following screw removal. The patient recovered without complications. Venous contact by pedicle screws should be treated on a case-by-case basis in a multidisciplinary approach with vascular surgery. We discuss a treatment algorithm for the operative management of this problem.
INTRODUCTION
Pedicle screws are used frequently in the treatment of numerous spinal pathologies [1]. Use of pedicle screws in thoracolumbar surgery is relatively safe, but complications can occur in which vascular involvement is rare [2]. Prior studies have reported vascular complications, which mostly occur in arterial vasculature, but reports of complications in the venous system are infrequent [3]. We describe a case in which pedicle screws were incidentally found to be in contact with both the inferior vena cava (IVC) and the right common iliac vein and discuss management pathways.
CASE REPORT
A 62-year-old female presented with low back pain. She had a prior history of a work-related injury that led to lumbar spinal fusion of L4–L5 at an outside hospital. She had some improvement in symptoms following the revision surgery, but continued to experience back pain and sought neurosurgical evaluation in our clinic. Physical exam was notable for 5/5 strength in the lower extremities bilaterally with normal patellar and Achilles reflexes. CT of the lumbar spine was concerning for the right L5 screw abutting the vasculature, so a CT angiogram and CT venogram of the abdomen were obtained (Fig. 1).

CTV showing right L5 screw (red arrow) indenting right common iliac vein.
The venogram demonstrated that the tip of the right L4 screw slightly indented the IVC and the right L5 screw moderately indented the right common iliac vein. After discussing the results with the patient, a plan was made to undergo surgery for removal of hardware, with vascular surgery present in case bleeding from venous injury was encountered after hardware removal.
During the procedure, the patient was placed supine and a venous sheath was placed in the right femoral vein by vascular surgery. After turning the patient to prone position, the sheath was secured away from the hip bolster with tape to assure the line remained unkinked and functional (Fig. 2). A prone venogram was taken, which showed the right sided hardware indenting the IVC and right common iliac vein. A small posterior lumbar incision was made 3.5 cm to the right of midline over the hardware, which was exposed via a Wiltse approach. The right sided screws and rod were removed (Fig. 3). After removal, bleeding through the pedicle screw tracts was not observed. With the patient still in the prone position, a venogram was taken immediately after screw removal and showed no extravasation of contrast. It also showed that there was no longer indentation on the IVC and the right common iliac vein (Fig. 4). Thus, no further intervention was required. The incision was closed and the venous sheath removed. The postoperative course was uncomplicated.

Venous sheath placed through right femoral vein (left). Planned incision line with venous sheath held in place by tape (red arrow) (right).

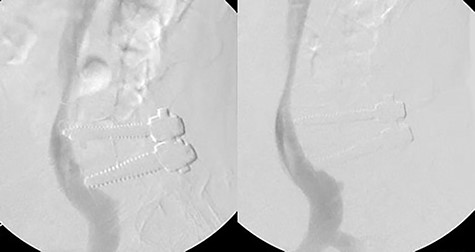
Venogram showing right hardware indenting right common iliac vein and IVC (left). Postoperative venogram displays indentation no longer present after hardware removal (right).
DISCUSSION
We describe a case of venous encroachment by pedicle screws. While arterial encroachment has been described in the literature frequently, reports on venous encroachment are much less common. Parker et al. described that 15 of 6816 placed screws had vascular contact, of which four were lumbar screws abutting the common iliac veins, while 10 were thoracic screws abutting the aorta [3]. Foxx et al. conducted a retrospective chart review on pedicle screws coming into contact with great vessels and found higher incidence of contact, with 33 of 680 screws coming into contact with vessels, and 22 of which were in contact with the iliac veins [4]. Discrepancies in these incidences could be due to institutional variation in the surgeon technique and skill. Another case report mentioned a lumbar pedicle screw that was pushed into the retroperitoneum intraoperatively and then migrated into the IVC, requiring endovascular retrieval [5]. Mirza et al. described a case wherein a left S1 screw was abutting the L5 nerve root and left common iliac vein [6]. With removal of the hardware, they also used intraoperative venogram to confirm the absence of vascular injury. They do not however describe a treatment algorithm for overall management of screw involvement in a venous structure.
In terms of management in our case, there was no extravasation upon removal of the hardware, and no evidence of vascular compromise with intraoperative venogram. Our treatment algorithm was defined preoperatively and we were prepared for other potential intraoperative findings. Had there been minimal contrast extravasation on the venogram, the surgical pathway would have remained the same, but postoperatively, the sheath would have been left in place and the patient would receive care in the ICU instead of a floor bed. In this situation, we believe the tissues in the retroperitoneum would likely tamponade a small amount of venous bleeding [7]. We would then repeat a venogram 24 hours later to verify that there was no contrast extravasation.
Had there been extensive extravasation on intraoperative venogram, the patient would have had a balloon placed through the venous sheath to tamponade the bleeding. The lumbar incision would be quickly closed, and the patient would be turned supine for a transabdominal open repair of the vein. While placement of an endovascular stent was discussed as a treatment option, long-term venous patency following stenting is a major issue. As such, endovascular stenting is used sparingly for cases of iliac vessel trauma [8, 9].
In the majority of cases, these patients are asymptomatic and the indication for screw removal is not well defined. Foxx et al. followed nine patients who had vascular contact by pedicle screw and found no sequelae as a result of vascular contact. They recommended considering risks and benefits of revision surgery in an asymptomatic patient [4]. Parker et al. concluded that only 2 of the 15 cases in their series of pedicle screw contact with vessels required revision [3]. Our patient had back pain unrelated to the venous contact and incidentally was found to have encroachment by the pedicle screws on the venous structures. After discussing the problem with the patient, she became very concerned about long-term risks to the vasculature and opted for screw removal. As the literature on these cases is sparse regarding risks and benefits of intervention, screw removal needs to be done on a case-by-case basis. We offer management pathways if surgery is pursued and encourage a multidisciplinary approach with vascular surgery.
ACKNOWLEDGEMENTS
We thank Walter Dent, Department of Neurosurgery, Tufts Medical Center, for acquisition of photos and other media related to the case.
Conflict of interest statement
None.



