-
PDF
- Split View
-
Views
-
Cite
Cite
Leshae A Cenac, Philip Xiao, Armand Asarian, Incidental discovery of mucinous adenocarcinoma from a suspected inflammatory perianal mass, Journal of Surgical Case Reports, Volume 2020, Issue 2, February 2020, rjz413, https://doi.org/10.1093/jscr/rjz413
Close - Share Icon Share
Abstract
Mucinous adenocarcinoma is a rare tumor that may be associated with longstanding perianal fistulas. It represents 6.9% of all anal cancers. The diagnosis of this malignancy can be delayed because the symptoms experienced by people with the disease are usually attributed to the fistula and not to malignant transformation. As a result, the diagnosis of perianal mucinous adenocarcinoma in the setting of chronic perianal fistulas requires a high index of clinical suspicion and specific histological features.
INTRODUCTION
Perianal fistula is a common disease that affects 12.3 per 100000 men and 8.6 per 100000 women [1]. However, its malignant transformation into mucinous adenocarcinoma is rare and represents 6.9% of all anal canal cancers [2]. The diagnosis of adenocarcinoma in chronic fistulas can be delayed because the symptoms present are usually attributed to the fistula thus postponing the suspicion of the development of adenocarcinoma [3]. We present a case of mucinous adenocarcinoma in a female with a 5-year history of a recurrent perianal fistula. This case report serves to raise awareness of the relationship between the two disease entities in order to aid in early recognition and treatment.
CASE REPORT
A 44-year-old female with a chronic perianal fistula presented to the clinic with a left lateral perianal mass associated with perianal bleeding, discharge and pain. The fistula tract was biopsied in 2017 and showed detached pieces of squamous epithelium and endocervical gland tissue in a background of acute inflammatory exudate. Subsequent magnetic resonance imaging (MRI) of the pelvis showed extensive subcutaneousinfiltrative changes with the fistula extending from the left inguinal crease to the anus.
A computed tomography (CT) of pelvis with contrast in 2019 showed an 8 × 7.3 × 5.6 cm lobulated, hypodense structure within the subcutaneous tissues along the left gluteal cleft, inseparable from the left levator ani muscles and was reported to be of an unclear etiology. A MRI with and without contrast showed a 7.3 × 7.3 × 5.8 cm structure with peripheral rim enhancement within the subcutaneous tissues of the left gluteal cleft abutting the skin surface with intermediate T1 signal and heterogeneous but overall increased T2 signal. This mass was reported to be suspicious of an area of infected granulation tissue given the rim enhancement. Two fistulous tracts were visualized on MRI measuring 6 and 3 mm, respectively. Bilateral enlarged lymph nodes were identified as 1.7 cm in the short axis along with a mildly enlarged external iliac node measured as 1 cm in short axis. Colonoscopy was performed to rule out occult inflammatory bowel disease and the entire colon appeared normal.
Surgery was scheduled to excise the suspected inflammatory tissue. An elliptical incision was performed around the perianal mass until healthy tissue was encountered. A small portion of the suspected inflammatory tissue was directly budding the medial portion of the anal sphincter and was left in place to maintain continence.
Microscopic examination of the excised mass revealed skin infiltrated by a neoplasm with extensive extracellular mucin pools. Within the mucin pools, there were clusters and strips of malignant intestinal type epithelium. These morphologic features were diagnostic of a moderately differentiated mucinous adenocarcinoma (Fig. 1). The immunohistochemical stains showed that tumor cells were positive for CK7, CK20 and CDX2 while negative for CK5/6 and PAX8, supporting an intestinal phenotype (Fig. 2).
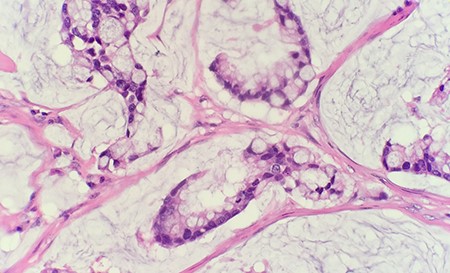
Microscopic examination reveals within the mucin pools are clusters and strips of malignant intestinal type epithelium (HE 40 × ).
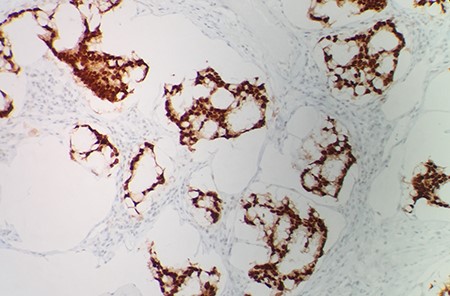
The immunohistochemical stain shows that tumor cells are positive for CDX2 (IHC 20 × ).
Bilateral excisional inguinal lymph node biopsy was performed, and both were positive for mucinous adenocarcinoma. Staging CT of the chest, abdomen and pelvis showed two nonspecific adjacent 3 mm left lower lobe pulmonary nodules and two sub-centimeter hypodense lesions in the right lobe of the liver that were too small to accurately characterize. Metastatic disease could not be entirely excluded.
DISCUSSION
Mucinous adenocarcinoma is a rare tumor that may be associated with longstanding perianal fistulas. While fistula associated adenocarcinomas are often seen in the setting of Crohn’s disease, they may arise in association with non-healing fistulas of other etiologies. Early diagnosis can be difficult because the tumor has a slow growth phase and does not pierce the rectal mucosa [4, 5]. The etiology of mucinous adenocarcinoma in a chronic perianal fistula is unclear and has been hypothesized to be due to either dysplastic degeneration in longstanding recurrent fistula or from seeding of granulating fistula by malignant cells arising from carcinoma of the colorectal mucosa [2]. Although this tumor has a low grade, it is usually diagnosed at an advanced stage and the diagnosis requires a high index of clinical suspicion and specific histological features such as the presence of mucin lakes and globules in the specimens collected from the perianal abscess [4, 5].
Our patient’s perianal mass was suspected to be inflammatory infiltrate secondary to either a long-standing perianal fistula or multiple corrective surgeries; malignancy was not suspected. This case is interesting because the patient’s perianal fistula was previously biopsied and did not show any changes that indicated mucinous adenocarcinoma. Within a 2-year period, a new, large perianal mass emerged and was identified on histology to be mucinous adenocarcinoma. Usually, it takes about 10 years for a perianal mucinous adenocarcinoma to arise from a chronic perianal fistula [6]. However, this patient had a cumulative 5-year history of a recurrent perianal fistula. Thus, indicating that there may be less time required for this malignancy to develop as compared with what the literature previously suspected.
Due to the rare progression of a chronic perianal fistula to a perianal mucinous adenocarcinoma, close observation of patients with long-standing perianal disease should be performed and a high index of clinical suspicion should always be maintained. Any longstanding perianal fistula should warrant the performance of multiple biopsies of the fistula tract [7], annual biopsies may be required. This could ensure that there is an early diagnosis and treatment of this malignancy since it does not have a specific clinical presentation that could alert the physician that transformation to carcinoma should be suspected [7].
Conflict of interest statement
There are no conflicts to be declared.
Funding
None.



