-
PDF
- Split View
-
Views
-
Cite
Cite
Yohei Kawatani, Atsushi Oguri, Hybrid repair of isolated internal iliac artery aneurysm, Journal of Surgical Case Reports, Volume 2020, Issue 2, February 2020, rjz409, https://doi.org/10.1093/jscr/rjz409
Close - Share Icon Share
Abstract
The best operation method for an isolated internal iliac artery aneurysm remains controversial. We report on a repair of an isolated internal iliac artery aneurysm. A 78-year-old man was referred to our facility for treatment of a left isolated internal iliac artery aneurysm. At first, we embolized the arteries distal to the aneurysm using coils and vascular plugs. Two weeks later, we performed open surgery. We resected the aneurysm wall through a transperitoneal approach only with proximal blood flow control and without surgical exposure and clamping of the arteries distal to the aneurysm. The blood flow of the internal iliac artery distal to the aneurysm had completely ceased after embolization in the first stage, which enabled us to avoid further pelvic dissection and potential bleeding. At the 6-month follow up, the patient was well and without complaints.
Background
The method for the operation of an isolated internal iliac artery aneurysm was first described by Maclaren [1] more than 100 years ago. However, the first-line treatment of this condition is still controversial to date. Endovascular stent-graft placement has become one of the standard treatment methods. Still, stent-grafting has limitations associated with the patient’s anatomy, and its long-term outcome is currently not clear. Therefore, open surgery is still an important option and widely performed.
On the other hand, in the case of aneurysms of the internal iliac artery, open surgery has an up to 7–11% higher mortality than endovascular therapies [2]. One of the main reasons for the unfavorable outcomes is bleeding during the operation [3].
We report a case of isolated internal iliac artery aneurysm that we successfully treated with a hybrid repair.
Case presentation
A 78-year-old man was referred to our facility for treatment of a left internal iliac artery aneurysm (36 mm in diameter on the left side) (Figure 1).
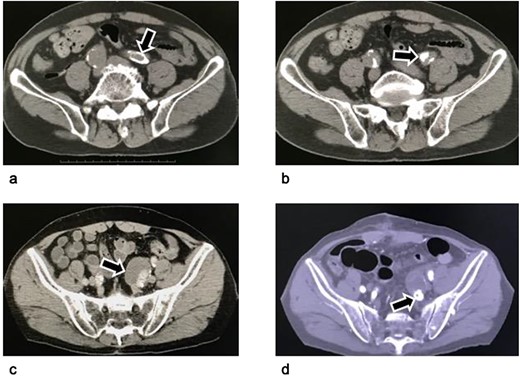
Computed tomography of an isolated internal iliac artery aneurysm. (a–c): Images before the operation: An isolated internal iliac artery aneurysm on the left with a diameter of 36 mm can be seen. The left common iliac artery and the neck of the left internal iliac artery aneurysm were severely calcified (arrows). (d) Image four months postoperatively: The aneurysm sac has become smaller because its wall was resected as much as possible. The vascular plug in the internal iliac artery is visible distal to the aneurysm (arrow).
We decided to perform hybrid therapy. In the first stage, we performed endovascular embolization of the distal branches of the left internal iliac artery aneurysm. We inserted a 5 Fr guiding sheath (Destination® Guiding Sheath, Terumo, Tokyo, Japan) into the left common femoral artery under local analgesia. The two branches distal of the internal iliac artery, that is the posterior and anterior divisions of the distal left internal iliac artery, were ebmolized. First, the posterior division was embolized with 3*60 mm, 4*80 mm, 6*100 mm and 8*20 mm microcoils (Interlock™ Fibered IDC Occlusion System, Boston Scientific, Marlborough, MA, USA). Ten-mm and 12-mm vascular plugs (Amplatzer™ Vascular Plug II, St. Jude Medical, Inc., Saint Paul, MN, USA) was deployed into the anterior division of the internal iliac artery and the internal iliac artery stem distal to the aneurysm (Figure 2). The patient was discharged without any complications and did not complain of buttock claudication.
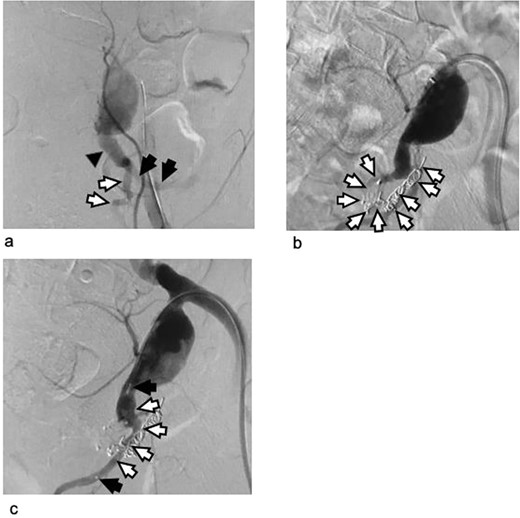
Arteriogram of the left internal iliac artery during the embolization procedure as the first stage of hybrid intervention. (a) Arteriogram before embolization: The left internal iliac artery stem distal to the aneurysm (black triangle) and the anterior (white arrows) and posterior division of the internal iliac artery (black arrows) are shown. (b) Arteriogram after coiling of the posterior division of the left internal iliac artery: Metal coils are visible from the posterior division of the left internal iliac artery to the superior gluteal artery. The microcoil was used because it provides good control in these narrow and tortuous arteries. (c) Arteriogram after vascular plug deployment: The left internal iliac artery stem and its anterior division were embolized using an Amplatzer vascular plug because they were wide and straight enough to insert the 5 Fr guiding catheter. Triangles: the vascular plug. The black arrows indicate the tip of the plug. The blood flow in the artery persisted after the plug had been deployed. The completion of embolization with metal devices needs time.
Two weeks later, we performed open surgery as the second stage of the hybrid procedure. We exposed the internal iliac artery through a median lower abdominal incision and transperitoneal approach. The neck of the internal iliac artery aneurysm was too short for clamping or ligation. We decided to clamp the common and external iliac artery instead to achieve proximal control. We then opened the aneurysm without having to take surgical control of the distal branches. There was no bleeding from the aneurysm. We closed the origin of the distal internal iliac artery with a 4–0 pledgeted suture. The shortness of the neck of the aneurysm and the calcification extending from the common into the external iliac artery did not allow us to ligate or directly close the origin of the artery. We therefore interposed a 7-mm Dacron artificial graft (J graft, Japan Lifeline Co., Ltd., Tokyo, Japan) between the common and external iliac artery for proximal repair (Figure 3).
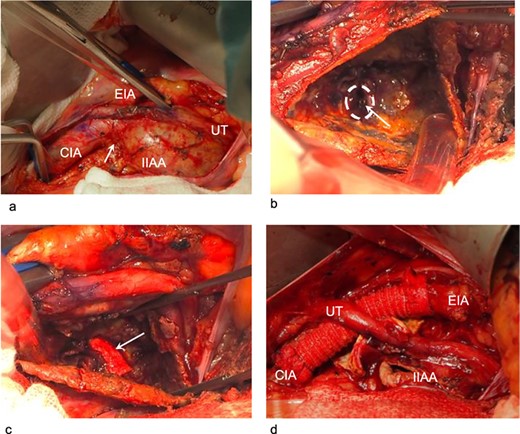
Intraoperative findings during the open procedure as the second stage of hybrid intervention. (a) Dissection of the vessels proximal to the internal iliac artery aneurysm: We clamped the common iliac artery and external iliac artery for proximal control. The neck of the internal iliac artery aneurysm was very short (arrow). (b) Without surgical clamping of the distal branches, we opened the aneurysm. The origin of the distal internal iliac artery and the tip of the vascular plug obstructing it are visible. No bleeding into the internal iliac artery aneurysm can be seen. The first-stage embolization had completely controlled the distal blood flow. Arrow: the tip of the vascular plug. Circle: the orifice of the internal iliac artery distal to the aneurysm. (c) We ligated the origin of the distal internal iliac artery with a 4–0 pledgeted suture to avoid dislodgement of the vascular plug and delayed bleeding. Arrow: one of the two pledgets used in the ligation. (d) The common iliac artery could not be directly closed. We interposed the artery for proximal repair. The aneurysm wall was resected as much as possible.
CIA: common iliac artery, EIA: external iliac artery, IIAA: internal iliac artery aneurysm, UT: ureter.
We resected the free wall of the aneurysm as much as possible and sutured the margins. The duration of the operation was 2.25 hours, and the blood loss was 70 mL. A red blood cell transfusion was not required.
At the 4-month follow up, the patient was well and without complaints.
Discussion
The isolated internal iliac artery aneurysm is relatively rare disease. The estimated incidence of an isolated internal iliac artery aneurysm is reported to be 0.3–0.5% of all intra-abdominal aneurysms [4]. Several treatment methods have been described for isolated internal iliac artery aneurysms, including ligation, excision, endoaneurysmorrhaphy, embolization, and endovascular stent-graft placement [2]. Endovascular stent-graft placement is reported to be safer than the open operation because it has a lower mortality and kidney dysfunction rate and entails less blood loss [5]. Manufactured branched stent-graft devices for the internal iliac artery are also reported to be effective and safe [6].
In this case, treatment with endovascular surgery only was technically possible but we assumed it was not the best option because the common and external iliac artery with the thrombus and calcification were not good landing zones and access rout for stent grafts. The diameter of the common iliac artery was too small for branched stent-graft devices. In addition, complications associated with the compression of surrounding organs by the remaining aneurysm sac have been reported after endovascular operations [5, 7].
On the other hand, open surgery for internal iliac artery aneurysms is naturally burdened with high mortality and blood loss as a result of the difficulty in gaining surgical control of the distal branches [3, 5]. It is challenging to expose the distal branches because they are located behind the aneurysm. The procedure is therefore associated with a potential injury to the pelvic veins [8].
After weighing the benefits and risks of both approaches, we chose hybrid therapy. In the first stage of the operation, we embolized the arteries distal to the aneurysm. This enabled us to avoid surgical exposure and dissection of the arteries distal to the aneurysm from the surrounding pelvic tissues. As a consequence, there was no bleeding even without surgical control of the distal branches during the open procedure in the second stage.
Among the material used for embolization, we can use either gelatin sponge or n-butyl-2 cyanoacrylate. These materials embolize vessels independent from a patient’s coagulation function and complete the earlier completion of embolization than with metal coils. However, gelatin sponge is reported to result more often in recanalization than other materials [9]. The embolization with n-butyl-2 cyanoacrylate is more difficult to control than other materials and, even though the incidence is low, there are reports on accidental distal embolization leading to ischemic injury [10]. Therefore, we used metal coils and vascular plugs. In addition, we put longer interval between endovascular embolization and open repair for completion of embolization.
With regard to the second stage open surgery, Chandra et al. [8] reported on the embolization of the distal branches for the first stage and proximal neck ligation for the second stage in an internal iliac artery aneurysm hybrid repair. While we had planned this procedure, we found intraoperatively that the proximal neck was very short, and the walls of the common iliac and external iliac artery were considerably calcified. The ligation of the neck or closure of the origin of the internal iliac artery were therefore not the best options, and we instead decided to interpose a Dacron graft between the common and external iliac artery for proximal repair. In addition, to avoid dislodgement of the vascular plug, we opened the aneurysm and ligated the origin of the distal branch.
Conflict of interest statement
None.
Funding
None.
Patient Consent
Consent to publish was obtained from the patient.
ACKNOWLEDGEMENTS
The authors are grateful to Akari Tajima, Kotomi Takahashi, Shinya Watanabe and Tomomi Fukuda for their help and support in the patient care and data analysis.



