-
PDF
- Split View
-
Views
-
Cite
Cite
Yaying Eileen Xu, Rasika Hendahewa, A rare case of mesenteric heterotopic pancreas presenting as an inflammatory mass, Journal of Surgical Case Reports, Volume 2020, Issue 2, February 2020, rjz395, https://doi.org/10.1093/jscr/rjz395
Close - Share Icon Share
Abstract
Heterotopic pancreas (HP) is a rare condition, is commonly asymptomatic and found incidentally at autopsy or during abdominal surgery. HP is usually found in the upper gastrointestinal tract, particularly in the stomach, duodenum and jejunum. Mesenteric heterotopic pancreas (MHP) has been rarely described in the literature, and there has been no reported case under ten years of age. We report a unique case of a 7-year-old African boy who presented with clinical appendicitis and intraoperatively was found to have a necrotic nodular mass in the jejunal mesentery which required segmental small bowel resection. Histology revealed mesenteric heterotopic pancreas with normal pancreatic tissue. As pre-operative diagnosis of MHP is difficult; we encourage a heightened awareness of this condition as a differential diagnosis in children presenting with abdominal pain and an inflammatory mass, which will subsequently aid in the management of these patients.
Introduction
Heterotopic pancreas (HP) is uncommon. It is a congenital malformation of the pancreas which lacks communication with normal pancreatic tissue [1]. It is usually found in the upper gastrointestinal tract—stomach (47%), jejunum (35%), duodenum (11.2%) and ileum (5.8%) [1]. Diagnosis of HP is often incidental; however, patients with HP can present with gastrointestinal bleeding, intussusception, abdominal pain or peritonitis secondary to perforation [2,3]. Mesenteric heterotopic pancreas (MHP), in particular, is even more rare with only very few cases having been described in the literature, and there has been no reported case under ten years of age [2,4]. We report a unique case study of a 7- year-old boy who presented with abdominal pain and an inflammatory mass secondary to MHP, in addition to a literature review on this rare diagnosis.
Case Report
A 7-year-old boy of African descent presented to the Emergency Department with two days history of right lower quadrant abdominal pain associated with multiple episodes of non-bilious vomiting. He was otherwise well and had no significant medical history. He was clinically dehydrated with a mild tachycardia of 120 beats per minute and was afebrile. He was tender in right lower quadrant and suprapubic regions and had an elevated white cell count of 26 × 10^9. His abdominal ultrasonography study revealed a considerable amount of free fluid in the right iliac fossa, and the appendix was not visualized. Given his age and the clinical picture, the most likely diagnosis was appendicitis and proceeded to theatre without further imaging.
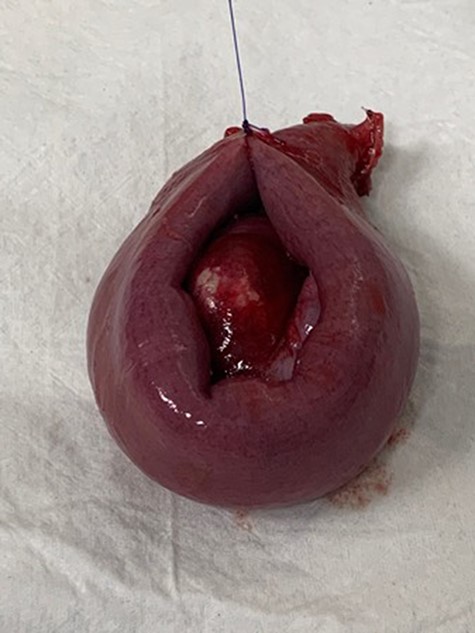
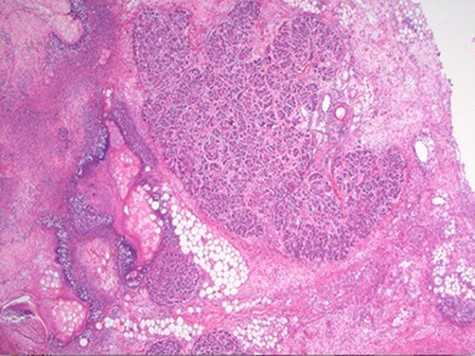
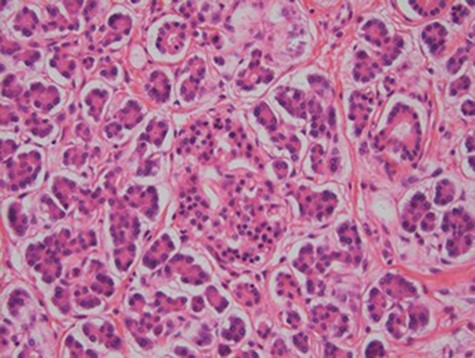
At laparoscopy, there were very dilated and inflamed loops of small bowel, and the appendix appeared normal macroscopically. Due to the extent of bowel dilatation obscuring adequate laparoscopic vision and assessment, decision was made to convert to an open procedure. At laparotomy, there was a nodular mass in the jejunal mesentery measuring about 3 cm in diameter with central necrotic tissue (Fig. 1). As it was adherent to the surrounding bowel, a limited small bowel resection was performed (Fig. 2) with side to side stapled anastomosis. Histology revealed normal small bowel wall with a mesenteric nodular mass comprised of architecturally normal pancreatic tissue including exocrine ducts and endocrine islets of Langerhans (Figs 3–5), consistent with a diagnosis of mesenteric heterotopic pancreas. His post-surgical recovery was uneventful and was discharged after five days of stay in hospital. He had an outpatient magnetic resonance imaging (MRI) of the pancreas which reviewed normal pancreas tissue, and he was followed up three months post-surgery.

Intraoperative finding of an inflammatory mass in the mesentery of jejunum with necrotic centre.
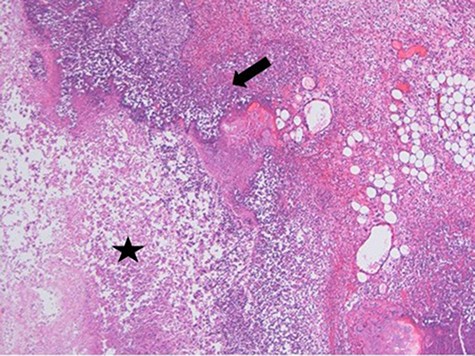
Necrosis (star) and acute inflammation with the presence of stromal neutrophils (arrow) within the mesenteric mass (H&E stain, x100).
Discussion
Heterotopic pancreas was first described by Jean Schultz in 1729 and histologically confirmed by Klob in 1859 [1]. One proposed theory is that during the development and rotation of the foregut and fusion of the ventral and dorsal buds of pancreas, small islands of pancreatic tissue are separated and continue to develop in the ectopic locations [3]. Mesenteric heterotopic pancreas in paediatric patients has been rarely described in the literature [4]. Most lesions are solitary, ranging from 0.2 to 5 cm and commonly composed of all components of the normal pancreatic tissue [1]. Most cases of HP are found incidentally during upper abdominal surgery and imaging or at autopsy. However, depending on the location, size and involvement of the structure, patients can present with symptoms secondary to pancreatitis, bowel obstruction, bleeding, intussusception, perforation and malignancy [1,2]. In this case report, the 7-year-old boy presented with severe abdominal pain which mimicked appendicitis, and an inflammatory mass was found.
According to the Heinrich classification system, heterotopic pancreas consists of three anatomical variations [5].
Type 1: normal pancreas tissue containing acini, islets and ducts
Type 2: acini and ducts, no islets
Type 3: only ducts are present.
Our patient had type 1 heterotopic pancreas, which is the most common type.
To date, there have been no cases of MHP in children younger than ten years of age [4]. Amongst the eight cases of MHP reported in the literature, 50% were aged between 12 and 15 years old, and the remaining 50% were adults [4]. It has been noted that there is a female predominance (6/8, 75%) of MHP, in comparison to the male predominance in HP. Most of the MHP cases have been found in the jejunal mesentery which was also evident in our patient [4].
The diagnosis of heterotopic pancreas prior to surgery is difficult due to its non-specific clinical signs and symptoms. Endoscopy is useful in diagnosing HP located in the stomach and first two parts of the duodenum. Imaging such as computed tomography (CT) and MRI may help in excluding other differential diagnoses. However, intra-operative surgical findings and subsequent histology would provide diagnostic confirmation of HP [6]. Surgical intervention is indicated when patients present with an acute abdomen, as did our patient who required segmental small bowel resection [1,5].
In conclusion, mesenteric heterotopic pancreas is extremely rare, and there has been no reported case younger than ten years of age in the literature. The management of MHP depends on the location and presentation, and surgical intervention maybe indicated when patients present with acute symptoms. It is important to have increased awareness and understanding of MHP, which plays an important role in the diagnosis and management of this rare condition.



