-
PDF
- Split View
-
Views
-
Cite
Cite
Eleni Effraemidou, Vasileios Souftas, Konstantinia Kofina, Michael Karanikas, Nikolaos Lyratzopoulos, Spontaneous rupture of a splenic artery aneurysm treated with a spleen-preserving procedure: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 2, February 2020, rjz412, https://doi.org/10.1093/jscr/rjz412
Close - Share Icon Share
Abstract
Splenic artery aneurysm is a rare and life-threatening condition, in case of spontaneous rupture. A rare case of such a rupture, treated successfully with an endovascular procedure, is presented. A 21-year-old man presented to the emergency department after an episode of loss of consciousness. After initial conservative treatment, he developed hemodynamic instability 12 hours later, with concurrent diffuse abdominal pain. Abdominal CT revealed a ruptured splenic artery aneurysm, which was immediately treated with coil embolization. The patient had an uneventful recovery and was discharged on the 12th day after the procedure. Although open surgery is the choice of treatment in cases of ruptured splenic artery aneurysms, endovascular embolization can also be considered a safe procedure with low complication and mortality rates.
Introduction
Splenic artery aneurysm is the most common visceral aneurysm, but is nonetheless a rare condition, with a prevalence of 0.1–2%, presenting a difficult diagnosis. It is defined as a dilatation of >1 cm of the vessel and is associated with portal or systemic hypertension, hormonal changes during pregnancy, fibromuscular dysplasia, intravenous drug abuse and other conditions; it can be classified as either true aneurysm and pseudoaneurysm [1]. It is usually diagnosed in patients >50 years of age and is four times more common in women [2].
Spontaneous intraperitoneal rupture is a life-threatening condition that can occur in 2–10% of cases, and it has a mortality rate of 40%. Open surgery still remains the gold standard for treatment of such cases; however, endovascular techniques have also gained acceptance because they have lower morbidity and mortality rates than open techniques [3].
We here present a case of ruptured splenic artery aneurysm in a 21-year-old male, with an initially misleading clinical condition. Endovascular embolization was the treatment of choice and had favorable results with no further complications.
Case Report
A 21-year-old male patient, with an uneventful medical history, came to the emergency department of our hospital after an episode in which he lost consciousness. The patient was hemodynamically stable, with blood pressure and heart rate within normal limits; ECG did not present any abnormalities, either. At the time of presentation, he was in a good neurological condition and did not mention any thoracic or abdominal pain. Blood laboratory investigation showed normal values of hemoglobin, hematocrit, glucose and other markers. He was then admitted to the department of internal medicine for further investigation.
Twelve hours later, the patient complained of diffuse abdominal pain, while a decrease of hemoglobin was observed (9.5 mg/dL), and hemodynamic instability presented, with an increase in heart rate to 100 bpm. He was initially treated with intravenous fluids; surgical opinion was then seeked. Clinical examination revealed pronounced rebound tenderness on all of the abdominal quadrants and decreased abdominal sounds. In order to investigate the possibility of intraperitoneal bleeding and considering the stability of the patient, an emergency abdominal CT scan with i.v. contrast was indicated. CT scan revealed the presence of a ruptured proximal splenic artery aneurysm measuring 26 mm × 18 mm, 6 cm from its origin (Fig. 1).
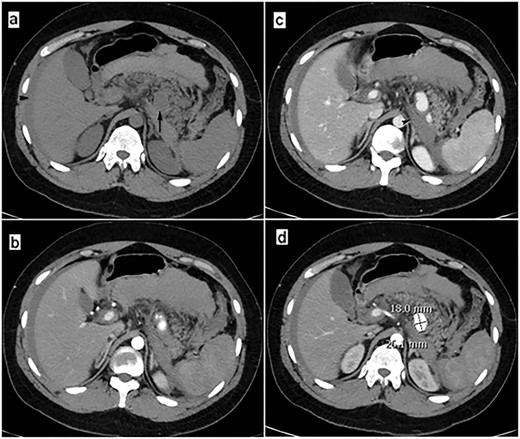
Abdominal CT scan at the onset of patient’s hemodynamic instability: (a) CT-image before the iv contrast administration shows the aneurysm (arrow) and free fluid (blood) into the infraperitoneal space and peritoneal cavity (arrowhead). (b, c and d) Post contrast CT-images (arterial phase) reveal the ruptured aneurysm clearly the free blood collection into the infraperitoneal space (arrowhead).
Thanks to the rather stable hemodynamic condition of the patient, and the fact that our institution is equipped to provide an endovascular approach, open surgery was excluded as the first therapeutic option; angiography with coil embolization of the aneurysm and proximal splenic artery was then performed. Under local anesthesia (injection of lidocaine solution 2%, Astra Zeneca, Athens, Greece), a percutaneous puncture of the right common femoral artery, and selective catheterization of the splenic artery was performed, using a 4-F Simmons 1 catheter (Cordis, Tipperary, Ireland). Subsequent angiography revealed the aneurysm, but an attempt to pass a microcatheter (Progreat®, Terumo, Leuven, Belgium) distally through the aneurysm failed. Embolization of the aneurysm itself and of the proximal splenic artery was decided, and 2D and 3D mechanically detachable fibered micro coils (Interlock-18, Boston Scientific, Cork, Ireland), and N-butyl-cyanoacrylate (NBCA) glue (Histoacryl®, Brown, Hessen, Germany) were used, preserving all of the collateral vessels for the spleen.
After embolization, the patient was stabilized and no signs of abdominal bleeding were observed on imaging. He was then transferred to our surgical department for further intense monitoring and treatment with intravenous fluids and blood transfusions. His recovery remained uneventful, as he did not develop further bleeding. He was discharged on the 12th day after the embolization in good condition; follow-up examination on an 8th-month basis showed preservation of the spleen, complete elimination of aneurysm and no other abnormal findings (Fig. 2).
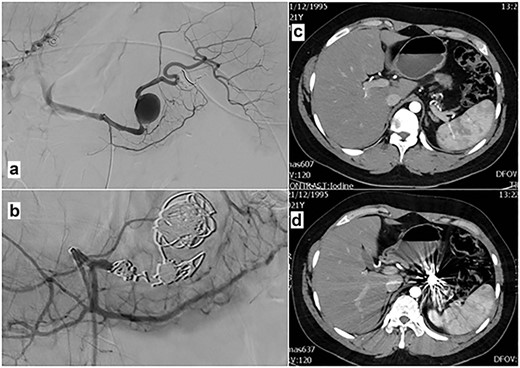
Angiography after selective catheterization of the splenic artery (a) reveals the ruptured aneurysm. Angiography after the micro coil and glue embolization of the aneurysm and the proximal splenic artery (b) shows complete obstruction of the lumen. (c and d) Post contrast CT-images (arterial phase) 8 months after splenic artery aneurysm embolization, show complete elimination of aneurysm and preservation of the collateral arteries to the spleen.
Discussion
Splenic artery aneurysm is the most common visceral artery aneurysm. It can remain asymptomatic and be diagnosed as an incidental finding; however, increases in its size, especially above 2 cm in diameter, increase the risk of rupture [4]. This can cause hemodynamic instability and abdominal pain, findings that our patient did not initially show, which led to delayed diagnosis. Other symptoms include nausea, vomiting, upper or lower gastrointestinal bleeding and anemia [5].
While open surgery remains the gold standard for treatment, a recent multi-center study on trans-catheter arterial embolization showed that only 6% of the patients presented complications such as acute pancreatitis, splenic infarction, abscess or intraperitoneal hematoma, and there was no in-hospital mortality [6]. The endovascular approach can be the fastest way to stop the bleeding, because it presents splenic ischemia through revascularization by collateral branches [7].
Endovascular approach includes coils, bare or covered stents, NBCA and the Amplatzer vascular plug, with or without maintenance of parent artery flow [8]. In our case, proximal and distal occlusion was necessary in order to prevent any backflow bleeding through collateral vessels.
Embolization success rates range from 55% to 100%, but complications can occur, such as post-embolization syndrome, splenic and intestinal infarcts, abscesses and migration of the embolization material. Anatomic characteristics, such as a short wide neck, and small diameter or tortuosity of the vessel can also compromise the use of these techniques [9]. However, splenectomy, with the subsequent risk of infections and overwhelming sepsis with high mortality, can be thus avoided.
In conclusion, endovascular treatment for ruptured splenic artery aneurysm is a safe and feasible procedure that can be performed immediately under local anesthesia, and it is considered gentler compared to open surgery. Even though open technique is still considered the gold standard, endovascular techniques could be preferred depending on the patient’s condition, anatomic characteristics and on medical expertise.
Conflict of Interest Statement
The authors have no conflict of interest to declare.
Authors’ contributions
E.E., V.S. and N.L.: description of patient’s treatment; K.K. and M.K. bibliographic research; K.K. drafted the manuscript. All authors critically revised the manuscript, approved the final version to be published and agree to be accountable for all aspects of the work.
Funding
None.



