-
PDF
- Split View
-
Views
-
Cite
Cite
Dante C Dali, Satvik Jhamb, C Steven Powell, Shahab A Akhter, Combined surgical treatment of symptomatic carotid, coronary and mesenteric occlusive disease, Journal of Surgical Case Reports, Volume 2020, Issue 2, February 2020, rjz392, https://doi.org/10.1093/jscr/rjz392
Close - Share Icon Share
Abstract
The surgical management of advanced symptomatic atherosclerotic disease in multiple distributions including the coronary circulation presents unique challenges due to the high risk of perioperative ischemic complications in the setting of coronary artery bypass grafting. We present a novel case of the combined surgical management of symptomatic carotid, coronary and mesenteric ischemic disease. The patient underwent carotid endarterectomy followed by combined coronary and mesenteric revascularization using cardiopulmonary bypass during the same hospital admission. He had an uncomplicated post-operative course and was discharged to home on post-operative day 7 after the combined procedure. Ninety-day follow-up was also unremarkable with the patient having no recurrent symptoms of ischemia. This case demonstrates the feasibility and safety of our approach for this rare clinical presentation.
Introduction
There is significant experience with combined carotid endarterectomy and coronary artery bypass grafting for symptomatic internal carotid and coronary artery disease. The outcomes of this operation have higher rates of neurological and other complications compared to each operation done in isolated fashion [1–3]. Two cases of combined surgical coronary and mesenteric revascularization have been reported for the extremely rare scenario of severe mesenteric and coronary artery disease [4,5]. We present a challenging case of a patient who presented with severe symptomatic carotid, coronary and mesenteric atherosclerotic disease with indications for surgical revascularization to address each of these vascular territories.
Case Report
The patient is a 58-year old male who was being evaluated for inguinal hernia repair. His past medical history included CAD with prior stenting of the left circumflex artery, diabetes with a HbA1c of 5.7 and an 80-pack year smoking history. He reported a 37 kg unintentional weight loss over 6 months with postprandial abdominal pain and nausea. In addition, he had exertional angina relieved by rest and sublingual nitrates. He had an abdominal CT scan for evaluation of the hernia, and this demonstrated severe atherosclerotic abdominal aortic disease with occlusion of the origin of the celiac and superior mesenteric arteries and patency of the inferior mesenteric artery. This was confirmed by mesenteric angiography which demonstrated occlusion of the celiac and SMA with a large mesenteric collateral originating from the inferior mesenteric artery (Fig. 2). This artery had a 90% orifice stenosis. With his cardiac history and symptoms, he underwent coronary angiography, which demonstrated significant left main and 3-vessel CAD (Fig. 1A and B). Left ventricular function was preserved with no valvular heart disease by transthoracic echocardiography.
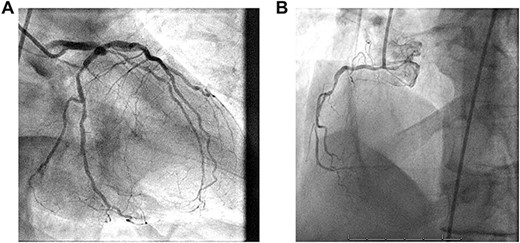
(A) 1. Left main coronary artery: large caliber vessel with distal 60% stenosis. 2. Left anterior descending coronary artery (LAD): large caliber vessel with proximal 80% stenosis gives rise to diagonals and septals. 3. Left circumflex coronary artery: large caliber, nondominant gives rise to OM 1 with proximal 70% stenosis before continuing with mid LCx 75% stenosis and distal 40% lesion. (B) Right coronary artery (RCA): medium caliber vessel that is dominant with proximal 85%, mid 85% and distal occlusion prior to PDA fills with left to right collaterals.

Mesenteric angiogram: both the celiac and superior mesenteric arteries are totally occluded, and the IMA provides the meandering mesenteric collateral. There was a 90% stenosis at the orifice of the IMA.
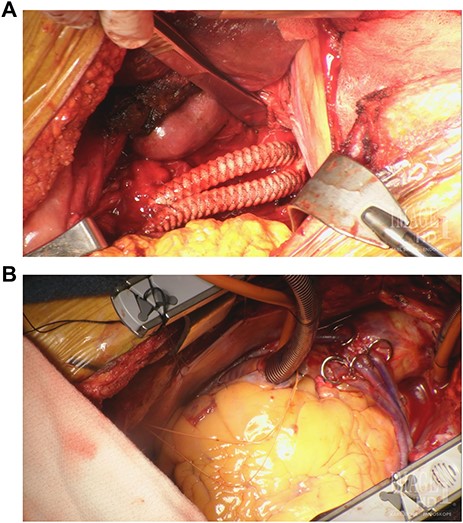
(A) Supra-celiac aorto-celiac and aorto-superior mesenteric bypass using a bifurcated Dacron graft. (B) CABG ×5 with proximal SVG anastomoses to the ascending aorta for D1, OM1, OM2 and PDA grafts. LIMA to mid-LAD graft not seen in this image.
He was referred initially for evaluation for coronary artery bypass grafting (CABG) and reported a brief episode of slurred speech in the past 2 months. A carotid duplex was obtained and showed 80–99% left internal carotid artery stenosis and 50–79% right internal carotid artery stenosis. Given his severe symptomatic carotid and mesenteric arterial disease, there would be significantly greater risk of neurological and mesenteric ischemic complications associated with CABG. The decision was made to perform surgical revascularization to address each vascular system in a staged and combined manner.
The patient underwent uncomplicated left carotid endarterectomy and was admitted postoperatively. He had no neurologic complications and was taken for combined CABG and mesenteric bypass on the fourth postoperative day. After induction of anesthesia and placement of hemodynamic monitoring lines, the procedure was initiated with a median sternotomy and mobilization of the left internal mammary artery as a pedicled graft. The greater saphenous vein was harvested endoscopically. After this was performed, a midline laparotomy was performed, extending the sternotomy incision. Dissection was carried through the lesser sac until the supra-celiac aorta was identified. The supra-celiac aorta, celiac artery and superior mesenteric artery were dissected from surrounding tissues. The patient was then systemically heparinized to achieve an activated clotting time (ACT) of greater than 450 seconds, and following aortic and right atrial cannulation, the patient was placed on cardiopulmonary bypass. Normothermic conditions were maintained. The mesenteric bypass was then performed from the supra-celiac aorta to the celiac artery and SMA with a bifurcated Vascutek® 12 mm × 6 mm Gelsoft™ graft (Terumo Cardiovascular Group, Ann Arbor, MI) in an end-to-end fashion (Fig. 3A). After completion of the mesenteric bypass, the patient was cooled to 34°C, and coronary artery bypass grafting was performed with saphenous vein grafts to the first diagonal, first obtuse marginal, second obtuse marginal and posterior descending coronary arteries followed by the left internal mammary artery graft to mid-left anterior descending artery (Fig. 3B). He was weaned from cardiopulmonary bypass without inotropic support. Total cardiopulmonary bypass time was 236 minutes (90 minutes for the mesenteric revascularization), and aortic cross clamp time was 125 minutes, using a single clamp technique. After administration of protamine, drains were placed and the sternum and laparotomy incision were closed. The patient had an uncomplicated course with return of bowel function on post-operative day 3 and was discharged home on day 7 from the combined procedure. The patient was seen in follow-up at 30 and 90 days post-operatively and had no recurrent neurological, cardiac or mesenteric symptoms.
Discussion
This patient presented a rare clinical scenario with severe symptomatic atherosclerotic disease in the carotid, coronary and mesenteric circulation. We felt that performing all three operations in a combined manner would carry a high risk, and therefore, the left carotid endarterectomy was performed first and without any neurologic, cardiac or mesenteric complications. The decision was made to combine the CABG and mesenteric bypass operations due to the potentially high risk of mesenteric ischemia in the peri-operative period with CABG alone and the risk of myocardial ischemia and dysfunction with the increased afterload associated with aortic clamping during the mesenteric revascularization. We addressed this issue by using cardiopulmonary bypass support for that part of the operation which preceded the CABG portion. The patient had no ECG changes or hemodynamic instability during the celiac and SMA bypass and there was no evidence of mesenteric ischemia manifested by metabolic/lactic acidosis during the CABG procedure.
Although this case represents a rare and complex clinical presentation, our timing and conduct of the cases and importantly the excellent outcome demonstrate one approach for handling symptomatic concomitant carotid, coronary and mesenteric arterial vascular disease.
Conflict of interest statement
None declared.
Funding
None.



