-
PDF
- Split View
-
Views
-
Cite
Cite
Shannon Greenberg, Jared C Inman, Esther Yung, Evelyn B Choo, Colon mass: a rare site of metastasis for squamous cell cancer of the head and neck, Journal of Surgical Case Reports, Volume 2020, Issue 2, February 2020, rjz391, https://doi.org/10.1093/jscr/rjz391
Close - Share Icon Share
Abstract
A 61-year-old man with a past medical history significant for heavy alcohol consumption and an extensive smoking history presented with a left neck mass which was diagnosed as a pT3N2bM0 squamous cell carcinoma (SCC) of the submandibular gland. The patient was later found to have recurrence with mediastinal metastasis despite adjuvant chemoradiation. He subsequently developed abdominal distention with computed tomography revealing an ascending colon mass and findings concerning for perforation. The patient underwent an exploratory laparotomy with right hemicolectomy. Surgical pathology was consistent with metastatic SCC.
Introduction
Cancer is the second leading cause of death in the USA with oral cavity, pharyngeal and laryngeal cancers accounting for ~3.7% of new cancer cases in the USA [1, 2]. Squamous cell carcinoma (SCC) accounts for nearly 90% of these head and neck cancers [2]. Major risk factors include tobacco and alcohol use as well as human papilloma virus, with a predilection for males in the fifth and sixth decades of life [3, 4]. Salivary gland neoplasms account for only 3–4% of head and neck cancers with 0.9–4.7% of salivary gland neoplasms attributable to SCC [4, 5]. SCC of the submandibular gland accounts for only 2% of malignant salivary gland tumors [4]. The most common sites for metastatic spread of cancers of the head and neck include the lungs and bones with infrequent hepatic and brain metastasis [3]. Metastatic spread of SCC from the head and neck to the colon is a rare event requiring further investigation.
Case Report
The patient is a 61-year-old man with a heavy smoking and alcohol history, who presented to a head and neck surgeon for the evaluation of a left neck mass that had been present for 18 months with interval increase in size. The mass was hard, non-tender, with fine needle aspiration demonstrating a cT2N0 atypical squamous lesion of the submandibular gland. The patient underwent radical excision with modified radical neck dissection and partial parotidectomy. The resulting pathology was consistent with moderately to poorly differentiated SCC with focal perineural invasion (pT3N2bM0). The patient underwent post-operative chemoradiation but presented within 1 year with local regional recurrence. He again underwent chemoradiation with radical excision of facial cancer with radical parotidectomy, left radical neck dissection and facial reconstruction (Figs 1 and 2).
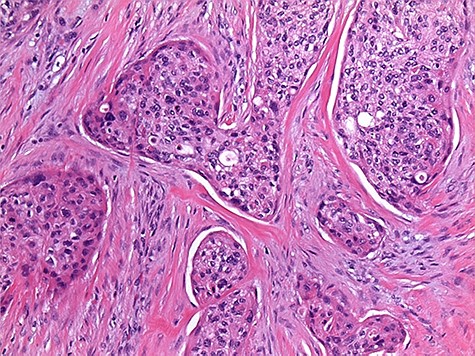
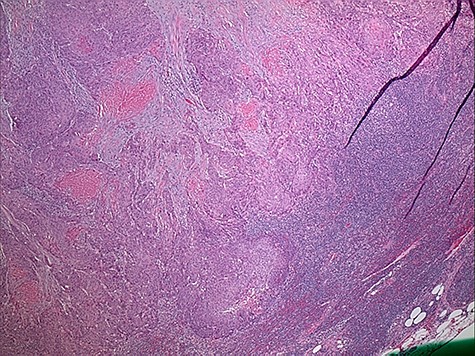
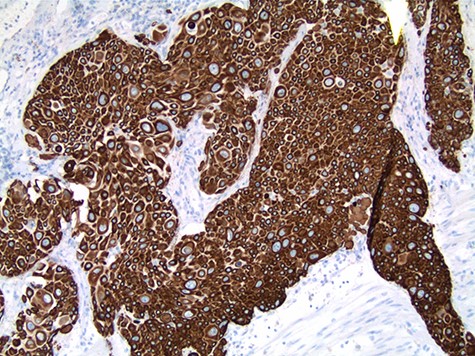
The patient’s post-operative course was complicated by dysphagia requiring gastrostomy tube placement. Surveillance imaging of the chest showed extensive mediastinal, hilar and supraclavicular lymphadenopathy with new pulmonary nodules and a large mediastinal mass encasing the trachea and ascending aorta consistent with distant metastatic disease. Cardiothoracic surgery was consulted and deemed the mass unresectable. On subsequent follow up, the patient endorsed a 2-year history of melena and was referred to gastroenterology for colonoscopy. However, prior to the scheduled colonoscopy, the patient was found to have abdominal distention with imaging confirming colonic pneumatosis and a large mass in the ascending colon. The patient’s clinical condition deteriorated despite non-operative management. He underwent exploratory laparotomy with right hemicolectomy, transverse colectomy and end ileostomy. Pathology workup included concurrent comparison of the salivary gland and colonic tumors, which showed similar histologic features. p63 and CK5/6 immunohistochemistry stain positivity in the colonic tumor confirmed the presence of SCC. CK20 and CDX2 immunostains to exclude a colonic primary adenocarcinoma or adenosquamous carcinoma were negative. In addition, due to the unusual initial presentation of a squamous appearing tumor in the submandibular gland, a MAML2 (11q21) rearrangement FISH study to rule out mucoepidermoid carcinoma (with squamous predominating features) was performed and was negative (Figs 3 and 4).

Discussion
Primary SCC of the submandibular gland is a rare tumor and like all head and neck SCCs has a predilection for older males with a history of smoking and/or alcohol consumption [3]. The traditional route of metastasis is to the local regional lymph nodes with distant metastasis to the lungs and bones, and occasional spread to the liver or brain [3]. Our patient demonstrates an unusual location for metastasis of a head and neck SCC. There are documented case reports of primary colonic SCCs as well as reports of metastatic spread of cervical and pulmonary SCC to the colon [6–8]. There is one case report of a synchronous metastatic SCC to the colon as well as the cervical lymph nodes from an unknown primary tumor [9]. However, this is the only reported case, to our knowledge, of a metastatic SCC to the colon from a primary submandibular SCC. The incidence of SCC of the colon is 0.1–0.27 per 1000 cases of colorectal cancer [6]. SCC of the colon is either primary or metastatic in origin. Differentiating between these two entities is important as metastatic SCC often has a worse prognosis [7]. Surgical excision and debulking are the primary treatment modalities though there is no standard regimen for treating metastatic SCC of the colon as these are very rare tumors [10].
This case highlights a rare primary tumor of the head and neck with an unexpected site of metastasis. Consequently, in patients who present with a colon mass in the setting of a known primary head and neck SCC, metastatic disease should be included in the differential diagnosis with prompt surgical intervention when appropriate.



