-
PDF
- Split View
-
Views
-
Cite
Cite
Hajar Bechri, Sidi Mamoun Louraoui, Meriem Fikri, Nizare El Fatemi, Moulay Rachid El Maaqili, Najia El Abbadi, Persistence of a trigeminal artery associated with a posterior meningeal artery aneurysm: case report and literature review, Journal of Surgical Case Reports, Volume 2020, Issue 2, February 2020, rjz389, https://doi.org/10.1093/jscr/rjz389
Close - Share Icon Share
Abstract
A 59-year-old female presented with severe headache and trouble of consciousness. The CT showed a subarachnoid hemorrhage FISHER IV with a hematoma of the right cerebellum. The angiography discovered a persistent left trigeminal artery associated with an aneurysm of the right posterior meningeal artery. The attempt of embolization failed and the patient suffered cerebral vasospasm and died. The persistence of a trigeminal artery is found in 0.1–0.6% of the population. It is the most frequent embryological carotid-vertebral anastomosis. It appears at the fifth week of development and disappears when the embryo reaches 5–7 mm. This embryological persistence is associated with numerous vascular abnormalities. The literature review showed the presence of those aneurysms in the trigeminal artery itself or the communicating artery. The association that we described is the first to our knowledge. Therefore, this association is particular and interesting to expose.
INTRODUCTION
The persistence and failure of involution of the embryonic communications between the anterior and posterior cerebral circulation contribute to vascular anomalies in adults. These carotid-basilar anastomoses are represented by: the primitive trigeminal artery, the primitive hypoglossal artery and the proatlantal artery with the trigeminal artery being the most common persistent anastomosis (0.1–0.6%) [1].
These embryonic communications usually present incidentally and may be associated with other vascular anomalies such as aneurysm formation revealed by sub arachnoid hemorrhage [1].
We report the first case of a persistent primitive trigeminal artery with a posterior meningeal artery (PMA) aneurysm.
CASE REPORT
We report a case of a 51-year-old female with no medical history presented for sudden severe headache radiating down her neck associated with nausea, vomiting and photophobia, followed shortly by unconsciousness. On the admission, she scored nine on the Glasgow coma scale with no motor deficit. Cranial computed tomography (CT) performed at admission revealed a sub arachnoid hemorrhage with a nonsurgical right cerebellar hematoma and no intraventricular hemorrhage not indicating an external drainage (Fisher IV) (Fig. 1).
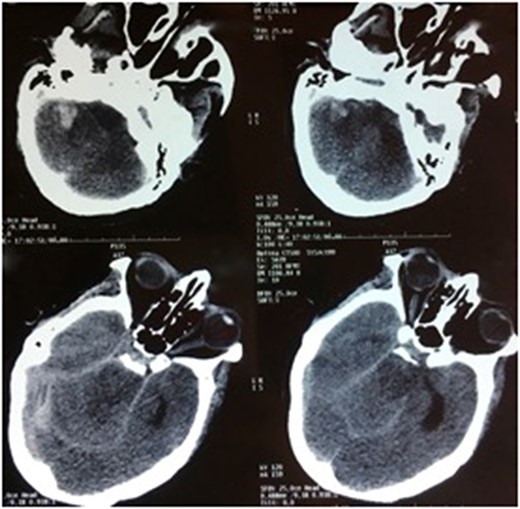
CT scan, axial sections, showing a FISHER IV subarachnoid hemorrhage with a right cerebellum hematoma.
The angiography concluded to a persistent left trigeminal artery associated with a medious saccular aneurysm (4.8 × 4.6 mm) originating from a right posterior meningeal artery (Fig. 2).
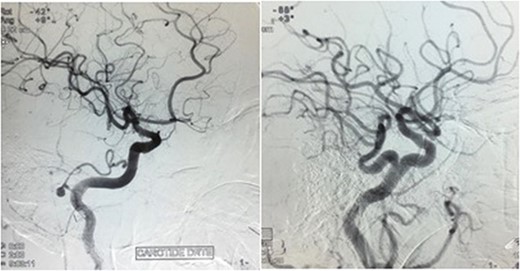
Angiography showing medious saccular aneurysm (4.8 × 4.6 mm) taking origin from a PMA with the persistence of a left trigeminal artery.
An attempt of embolization had initially failed and the patient manifested severe cerebral vasospasm that was resistant to intravascular medication. She was transferred to the intensive care unit and died before we could organize a second attempt of embolization.
DISCUSSION
The persistent trigeminal artery (PTA) was first reported at autopsy by Richard Quain in 1844 and via angiography by Sutton in 1950 [1]. With a frequency of 0.1–0.6%, it represents the most common persistent communication between the internal carotid artery (ICA) and the ventral bilateral longitudinal neural arteries, with a proportion of 85–87% of these persistent anastomoses (Table 1) [1–3].
Review of the literature about the association of a persistent trigeminal artery and aneurysms
| Author . | Year . | Age . | Sex . | Clinical presentation . | MRA findings . | Treatment . |
|---|---|---|---|---|---|---|
| Maeshima et al. [9] | 1999 | 48-year-old | Male | Headache | PPTA, multiples aneurysms anterior circulation | Staged surgery (3 time) |
| Aguiar et al. [6] | 2011 | 53-year-old | Female | Headache | Aneurysm of the PPTA—basilar junction, aneurysm of the anterior communication complex | Endovascular coil |
| Behari et al. [8] | 2004 | 40-year-old | Male | Right hemiparesis and complete left third nerve palsy | Tortuous right PCoA with two aneurysms | Staged surgery (2 time) |
| Aronson et al. [10] | 2008 | 65-year-old | Male | Headache | Ruptured pseudo-aneurysm of PMA at it anomalous origin from the PICA | Surgery (exclusion of the PMA) |
| Our case | 2016 | 51-year-old | Female | SAH WFNS IV | PPTA, PMA aneurysm | Attempt endovascular coil |
| Author . | Year . | Age . | Sex . | Clinical presentation . | MRA findings . | Treatment . |
|---|---|---|---|---|---|---|
| Maeshima et al. [9] | 1999 | 48-year-old | Male | Headache | PPTA, multiples aneurysms anterior circulation | Staged surgery (3 time) |
| Aguiar et al. [6] | 2011 | 53-year-old | Female | Headache | Aneurysm of the PPTA—basilar junction, aneurysm of the anterior communication complex | Endovascular coil |
| Behari et al. [8] | 2004 | 40-year-old | Male | Right hemiparesis and complete left third nerve palsy | Tortuous right PCoA with two aneurysms | Staged surgery (2 time) |
| Aronson et al. [10] | 2008 | 65-year-old | Male | Headache | Ruptured pseudo-aneurysm of PMA at it anomalous origin from the PICA | Surgery (exclusion of the PMA) |
| Our case | 2016 | 51-year-old | Female | SAH WFNS IV | PPTA, PMA aneurysm | Attempt endovascular coil |
Review of the literature about the association of a persistent trigeminal artery and aneurysms
| Author . | Year . | Age . | Sex . | Clinical presentation . | MRA findings . | Treatment . |
|---|---|---|---|---|---|---|
| Maeshima et al. [9] | 1999 | 48-year-old | Male | Headache | PPTA, multiples aneurysms anterior circulation | Staged surgery (3 time) |
| Aguiar et al. [6] | 2011 | 53-year-old | Female | Headache | Aneurysm of the PPTA—basilar junction, aneurysm of the anterior communication complex | Endovascular coil |
| Behari et al. [8] | 2004 | 40-year-old | Male | Right hemiparesis and complete left third nerve palsy | Tortuous right PCoA with two aneurysms | Staged surgery (2 time) |
| Aronson et al. [10] | 2008 | 65-year-old | Male | Headache | Ruptured pseudo-aneurysm of PMA at it anomalous origin from the PICA | Surgery (exclusion of the PMA) |
| Our case | 2016 | 51-year-old | Female | SAH WFNS IV | PPTA, PMA aneurysm | Attempt endovascular coil |
| Author . | Year . | Age . | Sex . | Clinical presentation . | MRA findings . | Treatment . |
|---|---|---|---|---|---|---|
| Maeshima et al. [9] | 1999 | 48-year-old | Male | Headache | PPTA, multiples aneurysms anterior circulation | Staged surgery (3 time) |
| Aguiar et al. [6] | 2011 | 53-year-old | Female | Headache | Aneurysm of the PPTA—basilar junction, aneurysm of the anterior communication complex | Endovascular coil |
| Behari et al. [8] | 2004 | 40-year-old | Male | Right hemiparesis and complete left third nerve palsy | Tortuous right PCoA with two aneurysms | Staged surgery (2 time) |
| Aronson et al. [10] | 2008 | 65-year-old | Male | Headache | Ruptured pseudo-aneurysm of PMA at it anomalous origin from the PICA | Surgery (exclusion of the PMA) |
| Our case | 2016 | 51-year-old | Female | SAH WFNS IV | PPTA, PMA aneurysm | Attempt endovascular coil |
From an anatomic perspective, the PTA usually originates from the posterior or lateral surface of the intra cavernous ICA just proximal to the origin of the meningohypophyseal trunk. Sometimes it can arise more proximally from the ICA, before the proximal dural ring, and there are also reports of it branching from the petrous ICA. With a medial course, it passes between the posterior bend of the ICA laterally and the pituitary gland medially [3, 4].
In 1958, Georg-Fredrik Saltzman evaluated eight cases of primary PTA and classified it, according to the angiographic characterizes, into two major variants and a mixed type of those variants. In fact, he described [5, 6].
Type 1: the PTA enters the basilar artery (BA) between the superior cerebellar artery (SCA) and the anterior inferior cerebellar artery (AICA), and the vertebrobasilar system distal to the anastomosis is supplied by the PTA. In these cases, there was poor filling of the posterior communicating artery (PcomA), with the patients thus having the adult type of bilateral PCAs.
Type 2: the PTA enters the BA, but mainly supplies the SCAs bilaterally. In these cases, the PCAs receive blood flow through the PcomA.
Type 3: combination of the types 1 and 2.
Some authors have described the PTA variant as a cerebellar artery arising from the precavernous ICA without connection to the BA [3].
Because it is a bifurcation, the PTA itself can be a potential site of aneurysm formation. When located into the PTA, the aneurysm can arise from the bifurcation of the cavernous ICA segment and the PTA, on the PTA trunk itself, or at its junction with the BA [1, 5, 6]. Usually, the PTA aneurysms described were saccular; fusiform shapes were rare [1, 7].
Many cases of PTA were reported to be associated with intra cranial aneurysms. This high prevalence has been explained by haemodynamic flow changes that promote aneurysm formation [2]. Besides, in a recent analysis of a large number of MRA studies (over 16 000 patients), the frequency of intra cranial aneurysm coexisting with PTA was 4.2%, which is similar to the general population (3.7%) [5].
Many potential sites of aneurysm formation have been described: Behari et al. described the association of PTA with posterior communication artery aneurysm [8]; Maeshima et al. reported a case of PTA and multiple aneurysms originating from the anterior cerebral artery and the middle cerebral artery [9]. To the best of our knowledge, we report the first case described of an association of an incidental PTA with a PMA aneurysm. In fact, the patient presented with a WFNS 4, FISHER IV sub arachnoid hemorrhage revealing a ruptured PMA aneurysm at its anomalous origin from the AICA.
Indeed, the PMA normally arises from the V3 segment of the vertebral artery, at or just below the foramen magnum [10]. Anatomic variations of its origins, explained by the embryological development theories, have been described such as its variant origin from the PICA. Among the five cases described through the literature, only two were associated with vascular anomalies [10].
Thus, the PMA may arise from the AICA by persistence of an embryological channel with regression of the usual proximal channel from the VA [10]. The development of aneurysm may be explained by physical stress with haemodynamic flow changes. The PMA has multiple anastomoses with the arteries of the falx cerebri, including the middle meningeal artery and meningeal branches of the posterior cerebral artery leading to an abundant blood supply allowing the proximal PMA to be occluded surgically or by coiling [10].
Unfortunately, our patient manifested cerebral vasospasm and died before we could perform the exclusion by endovascular therapy.
CONCLUSION
The knowledge of the embryonic communications between the anterior and posterior cerebral circulation might help understanding some cases of sub arachnoid hemorrhage. This better understanding of the anatomy helps achieving a better treatment whether it is surgical or endovascular.
CONFLICT OF INTEREST
None declared.
FUNDING
None.



