-
PDF
- Split View
-
Views
-
Cite
Cite
Joshua Agilinko, Najam Husain, Daniele Fanelli, Syed Soulat Raza, Pradeep Kumar, When DVT turns into surgical catastrophe: undiagnosed case of May-Thurner syndrome leading to retroperitoneal haematoma and fatal bleeding, Journal of Surgical Case Reports, Volume 2020, Issue 2, February 2020, rjz385, https://doi.org/10.1093/jscr/rjz385
Close - Share Icon Share
Abstract
May-Thurner syndrome (MTS) is an unusual cause of deep venous thrombosis; even rarer is the spontaneous rupture of collaterals around the thrombosed common iliac vein due to MTS. We present a case of MTS which presented with left leg swelling and abdominal mass due to retroperitoneal haemorrhage.
INTRODUCTION
May-Thurner syndrome (MTS) is the symptomatic compression of the venous flow of the left lower extremity. Its true incidence remains unknown but has been found to be in the range of 22–32% in post mortem studies. Despite the high prevalence, its association with deep vein thrombosis (DVT) is 2–3% of all lower extremity DVTs [1, 2]. The pathogenesis of MTS is believed to be related to the transverse course of the left common iliac vein and the fact that it underlies the right common iliac artery whilst ascending to the inferior vena cava. As a result, it can be compressed between the artery on top and the fifth lumbar vertebrae at the bottom. The pulsation in the artery which overlies the left common iliac vein is presumed to cause elastin and collagen deposition along with intimal fibrosis leading to formation of venous spur and venous thrombosis [3]. MTS can further present as acute or chronic DVT leading to pulmonary embolism (PE), chronic leg pain, chronic ulcers, or skin pigmentation changes. Although the most common causes of bleeding from the iliac vein are secondary to penetrating/blunt trauma to the lower abdomen, spontaneous rupture is an even more unusual presentation. There are only a small number of reported cases in the literature of spontaneous rupture of the iliac vein [4, 5, 6].
CASE REPORT
A 60-year-old Caucasian female was referred by her GP for a 2-day history of pain and swelling of the left leg. On examination, there was obvious limb swelling and a mass in the left iliac fossa. Soon after the presentation, the patient became hypotensive and arrested requiring cardiopulmonary resuscitation (CPR). The initial working diagnosis was PE secondary to DVT. Baseline investigations were normal but arterial blood gases showed compensated metabolic acidosis. After resuscitation, an urgent CT of abdomen, pelvis and chest was organized; this confirmed DVT of the left common iliac vein and also a large left adnexal mass with minimal ascites (Fig. 1). The patient, evidently in hypovolemic shock, was transferred for urgent exploratory laparotomy. She was found to have a large retroperitoneal haemorrhage with blood welling from the region of left iliac vessels. Proximal and distal control of iliac artery and vein was gained by tape and clamps allowing perioperative hypotension to improve. The vascular surgeon was called for help from the nearest tertiary centre. Upon further dissection, in the presence of the vascular surgeon, bleeding was noticed around the left common iliac vein, coming from the severed collaterals; these were eventually controlled with 6/0 prolene sutures. As the source of bleeding was not very clear, an opinion from vascular radiologist was sought. Review of the CT suggested that bleeding was likely to represent spontaneous rupture of venous collaterals due to DVT in the left iliac vein, secondary to MTS (Fig. 2). The patient was transferred to ITU with plans for relook surgery in next 48 hours once she had recovered from the acute insult. Unfortunately, the patient died the next day due to multi-organ failure and DIC secondary to massive transfusion.
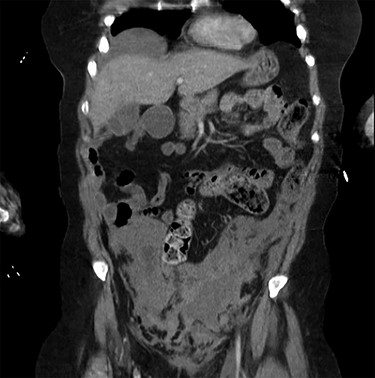
Coronal view of the CT scan showing the localized pelvic haematoma.
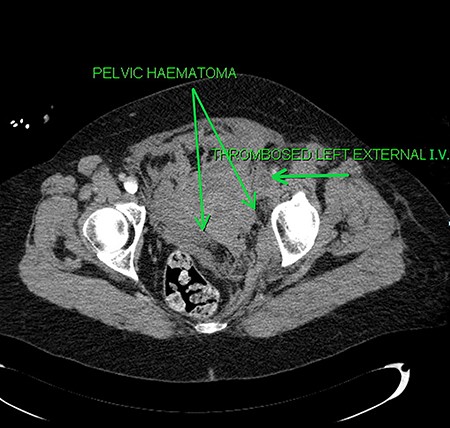
Axial sections of the CT scan showing the thrombosed external iliac vein (I.V.) and the pelvic haematoma.
DISCUSSION
There are several hypotheses for spontaneous rupture of the iliac vein. Venous hypertension triggered by an overlying thrombus or a Valsalva manoeuvre such as coughing, defecation, bending, or similar efforts has been the most frequently suggested predisposing factor [4]. Proximal venous obstruction by the overlying right common iliac artery or the endothelial spur could be a contributing factor [7].
Typically, the patients are predominantly middle-aged post-menopausal females; as a result, a popular hypothesis of hormonal effect has been suggested. Oestrogen induces relaxation of smooth muscle and softening of collagen fibres, which in turn increases distensibility of veins [8]. Falling oestrogen levels in this age group making veins less distensible and thrombophlebitis combined with a sudden rise in intraluminal pressure in a segment of the vein between the inguinal ligament and the right common iliac artery may be one of the possible explanations for the spontaneous rupture of the iliac veins [9].
Patients would usually present with hypovolemic shock due to the ongoing bleeding. Unfortunately, our patient ended up with the same presentation eventually requiring emergency exploratory surgery only to find an expanding pelvic haematoma the cause of which was the spontaneous bleeding from the left common iliac vein.
Most cases in the literature were operated under the misdiagnosis of a ruptured aortic aneurysm or an abdominal catastrophe due to a gynaecological problem. Thus, correct preoperative diagnosis is a prerequisite for resuscitation and correct surgical management.
In our case, we were unable to make a clear diagnosis pre-operatively even though the CT scan was done. The persistent hypotension and two cardiac arrests prompted a hemorrhagic source, and therefore the patient was transferred to the operating room prior to the CT being reported by the on-call radiologist. The exact reason for the trigger of bleeding remains unclear in our case.
The ideal course of treatment would be arresting the source of haemorrhage with direct suture, maintaining vascular continuity and the placement of an IVC filter to counteract the possibility of post-operative DVT in patients. This treatment has been suggested in the 17 cases with spontaneous rupture.
Possible surgical alternatives to direct suture are venous patch angioplasty and ilio-iliac crossover bypass reconstruction combined with a temporary arteriovenous fistula at the groin.
Conservative treatment can be an alternative in selected cases with no evidence of further bleeding, leg ischemia or impending venous gangrene [9].
O’Sullivan et al. [10] reported that endovascular management of MTS is safe and effective and may replace surgical reconstruction or anticoagulation alone.
CONCLUSION
Spontaneous rupture of the iliac vein is a vascular emergency that should be treated immediately. High clinical suspicion and CT scan play an important role in the correct pre-operative diagnosis. In middle-aged women presenting with left-sided retroperitoneal haematoma and DVT, this diagnosis should be considered. When MTS is associated, endovascular prosthesis combined with surgery can be another therapeutic option with an excellent result for the immediate cessation of extravasation and restoration of the venous patency.



