-
PDF
- Split View
-
Views
-
Cite
Cite
Sarah Bouayyad, Jen Ong, Houda Bouayyad, Heerani Woodun, Epiglottic granular cell tumour: a case report and literature review, Journal of Surgical Case Reports, Volume 2020, Issue 2, February 2020, rjaa009, https://doi.org/10.1093/jscr/rjaa009
Close - Share Icon Share
Abstract
Granular cell tumour is a rare, benign tumour that may arise in the soft tissues of various locations. It is often asymptomatic; hence, it gets misdiagnosed as other conditions. This is a case of an asymptomatic 50-year-old male with an incidental finding of a supraglottic lesion during routine oesophagogastroscopy. Examination under general anaesthetic showed a whitish non-ulcerating exophytic lesion on the laryngeal surface of the epiglottis, sparing anterior commissure and vocal cords. Surgical excision was performed with an open supraglottic laryngectomy approach. Histopathology confirmed GCT, strongly positive for S-100 protein and weakly positive for CD68. Accurate histologic analysis is a key to identify this rare tumour among other differentials. Although benign, ongoing monitoring is advised due to risk of recurrence.
INTRODUCTION
Granular cell tumour (GCT) is an uncommon neuroectodermal tumour that arises in soft tissues, predominantly in the oral cavity [1–6]; it may also arise in gastrointestinal tract [7–9], respiratory tract [9] and skin [9, 10]. GCT is usually benign and often asymptomatic, with malignant forms occurring in only 1–2% [1]. Despite this, histological features can be confused with squamous cell carcinoma (SCC) [3], leading to different treatment implications in laryngeal lesions.
We present a case of supraglottic GCT in a 50-year old man, which was an incidental finding on a routine oesophagogastroscopy.
CASE REPORT
A 50-year-old man presented for a routine oesophagogastroscopy to investigate for anaemia of unknown cause. He had a background of hypertension, mitral regurgitation, lower limb venous ulcer and alcoholic liver cirrhosis with known oesophageal varices. He was a smoker. He had no upper aerodigestive tract symptoms.
A laryngeal abnormality was noted, and he was referred to ENT for further assessment (Fig. 1). Flexible nasendoscopy showed a lesion on the laryngeal surface of the epiglottis in the midline. Vocal cords were not affected, although the lesion was extending close to the anterior commissure. An 18 × 14-mm lesion was found on magnetic resonance imaging (MRI) at the right paracentral supraglottic region, crossing the midline with possible involvement of the base of epiglottis (Fig. 2). There was no destruction of the thyroid cartilage or hyoid bone, and no involvement of the para-epiglottic space or glottis. There were no pathological cervical lymph nodes. Further CT scanning of the neck and chest confirmed the above, with no lung metastases identified (Figs 3 and 4).
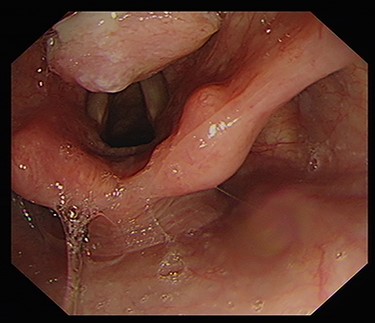
endoscopic image demonstrating ulcerative growth on the laryngeal surface of the epiglottis.
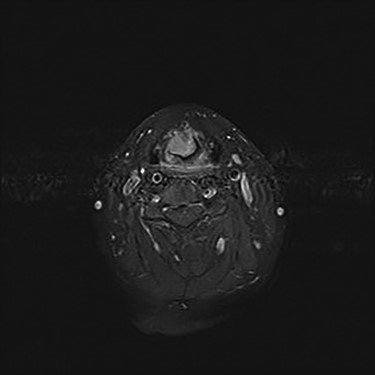
axial MRI T1FS with gadolinium image with 16 × 15 × 12 mm almost rounded well defined and enhancing lesion related to the base of epiglottis with no definite involvement of the tongue base.
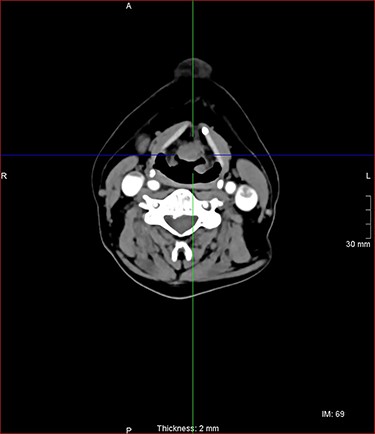
axial postcontrast CT images of the neck with similar lesion related to the base of epiglottis, no involvement of the pre epiglottic fat.

sagittal postcontrast CT images of the neck with similar lesion related to the base of epiglottis, no involvement of the pre epiglottic fat.
Further examination under general anaesthetic revealed a whitish, firm, non-ulcerating exophytic lesion. This was biopsied and debulked with coblation to good effect with a small remnant remaining in the midline.
Histopathological examination revealed large cells with granular eosinophilic cytoplasm and nuclei with scattered mild to moderate atypia. These cells expressed CD68, CD56 and S100, and lacked expression of AE1 and AE3. Focal spindling of cells was present with no obvious necrosis or mitosis. The squamous surface epithelium was orthokeratizing with mild pseudoepitheliomatous hyperplasia (Figs 5 and 6).
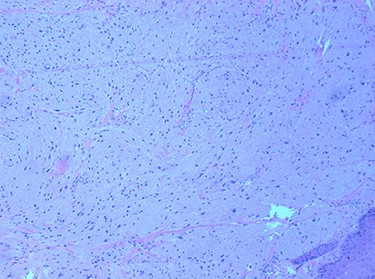
tumour cells with abundant granular cytoplasm and sub-epithelial proliferation. H & E 100×.
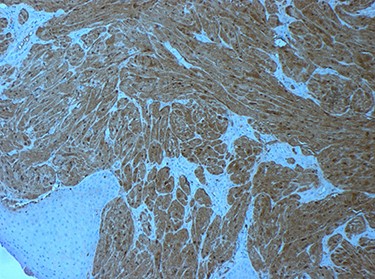
tumour cells staining positive for S-100 on immunohistochemistry.
As per local protocol, potential management options were discussed with the regional multi-disciplinary team (MDT). Although the histological features were not convincingly unfavourable, it was thought to be at worst an intermediate tumour. Surgical excision was recommended with an open supraglottic laryngectomy approach and temporary tracheostomy.
Intra-operatively, the tumour was noted to be close to but not involving the anterior commissure (3 mm clearance). The thyroid cartilage was marked for incision horizontally, with drill holes placed before incising to aid subsequent closure (Fig. 7). The central portion of the hyoid bone was also removed lateral to the lesser cornua. The remainder of the thyroid cartilage was sutured to the tongue base and vallecula. Arytenoids were preserved as well as much of the false cord mucosa. An additional sliver of tissue was taken and sent to histology as the final specimen was noted to be close to resection margins inferiorly.
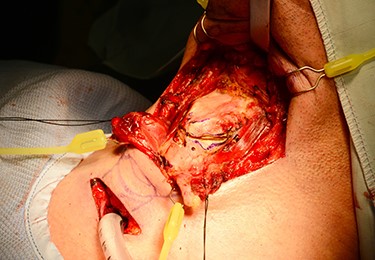
diathermy markings of thyroid cartilage before division. Note existing drill holes placed before resection to aid subsequent closure.
Macroscopically, the final specimen demonstrated a white submucosal epiglottic nodule (Fig. 8). Immunohistochemistry showed GCT (strongly positive for S-100 protein and weakly positive for CD68). Microscopically, tumour cells had abundant granular cytoplasm that was periodic acid-Schiff (PAS) positive and diastase resistant; these cells were closely associated with some nerve fibres. The tumour abutted the epiglottic cartilage. The closest margin was <1 mm inferiorly with good clearance (≥3 mm) at other mucosal margins. There was no evidence of necrosis, atypical mitoses or increased mitotic activity.

laryngeal surface of supraglottic laryngectomy—specimen for histology. Pale nodular lesion just to right of midline close to inferior margins.
Recovery was uneventful with decannulation of tracheostomy and commencement of oral intake at 7 days. Follow-up at 3 months confirmed gradual improvement of swallow with no signs of recurrence. His voice quality has stabilized. However, he does have some episodes of dysphonia. This would appear to relate to his intermittent coughing to clear saliva around the laryngeal inlet.
DISCUSSION
Accounting for less than 10% of GCTs of head and neck, laryngeal GCT is a benign tumour, which may mimic SCC [9]. As in our case, laryngeal GCT is usually asymptomatic [2, 3], but some cases present with dysphonia [1, 2, 4, 5, 9]. Most case reports of laryngeal GCT demonstrate involvement of the vocal cord [1, 2, 3, 5]. Our patient did not have vocal cord involvement and was asymptomatic.
GCT can be identified by histopathological studies using haematoxylin and eosin (H&E) staining, which shows polygonal, large cells clustered in nests or sheets with coarsely granular eosinophilic cytoplasm [5, 7–9]. Malignant GCTs are characterized by histologic features such as tumour necrosis, increased mitotic index and spindling of cells, but clinical behaviour such as metastasis must also be taken into account [9]. Immunohistochemical staining of GCT has been shown in the literature to be positive for S-100 protein [1, 3–10], PAS [7, 9, 10], neuron-specific enolase [3–7, 9], vimentin [5, 7] and CD68 [6, 7, 9, 10]. In our case, S-100 and CD68 were positive with PAS. The presence of pseudoepitheliomatous hyperplasia (reactive epithelial proliferation with pseudoinfiltrative growth pattern) is common in GCT and can be confounding in some instances, as it may be mistaken for well-differentiated SCC especially if small biopsies are taken [3].
Treatment for GCT is surgical resection with clear margins [2, 4, 9]. However, surgical clearance and technique can depend on the location of the tumour [2, 4] in order to minimize morbidity, for instance in laryngeal tumours where laryngeal competence can be affected. Techniques include CO2 laser [1–4] and cold-steel excision [4, 5]. Individualized management of patients with patient-centred MDT discussion usually leads to better outcomes [4]. For this case, transoral laser surgery was considered initially, but rejected due to the close extension of the lesion toward the anterior commissure. Thus, supraglottic laryngectomy was performed.
From an educational viewpoint, it is important to consider that GCT, which is a benign tumour, may be mistaken for SCC clinically and histologically. While rare, malignant forms of GCT do have poor prognosis [9]. Deep biopsies to facilitate an accurate histopathological diagnosis are paramount. Treatment is typically surgical resection depending on the anatomical location of the tumour. Ongoing monitoring is advised due to risk of recurrence.
ACKNOWLEDGEMENTS
We would like to thank the pathology and radiology department of Wythenshawe Hospital for kindly providing us details of histopathologic analysis as well as facilitating acquisition of relevant photomicrographs.
Conflict of interest statement
We declare no conflict of interest.



