-
PDF
- Split View
-
Views
-
Cite
Cite
Yi Liang, Angelina Di Re, Grahame Ctercteko, Iatrogenic rectal injury associated with fleet enema administration masquerading as Fournier’s Gangrene, Journal of Surgical Case Reports, Volume 2020, Issue 2, February 2020, rjz414, https://doi.org/10.1093/jscr/rjz414
Close - Share Icon Share
Abstract
Rectal injuries secondary to fleet enemas are the result of a chemical irritation as well as mechanical trauma causing localized perforation and mucosal necrosis. These injuries can be managed expectantly. Fournier’s Gangrene is a life-threatening, fulminant soft tissue infection of the genito-perineal region commonly secondary to a perianal infection, requiring extensive debridement of all affected tissue and judicious antibiotic therapy. This distinction is critical in the management of the current case, allowing for limited debridement and judicious observation without a resection of the injured rectum. A diverting colostomy allows for effective faecal management and minimizes contamination of the perineal wound.
INTRODUCTION
Fournier’s Gangrene (FG) is a life-threatening necrotizing, soft tissue infection of the perineum with a rapid clinical course [1–3]. FG is associated with precipitating colorectal pathology in up to 50% of cases [1]. Clinical evaluation and timely surgical debridement, aided by laboratory findings, are the mainstay of diagnosis. The role of radiology should not delay surgical intervention; however, it may assist in atypical presentations [1]. The initial treatment of FG requires aggressive local debridement of necrotic tissue and appropriate antibiotics [4]. Rectal enema injuries (REI) are a rare complication of enema administration, though rates of injury are underreported [5]. The pathophysiology is the combination of mechanical trauma to rectal mucosa by the device tip, overdistension of the rectum and chemical irritation secondary to the sodium phosphate found within Fleet® Enema (phospho-soda) (Fleet Co, Inc, Lynchburg, VA, USA) [5]. We present a case of FG superimposed upon an REI secondary to a fleet enema. We advocate for judicious debridement as a means for preserving the rectum.
CASE STUDY
A 51-year-old gentleman was admitted to hospital requiring an urgent neurosurgical intervention. The patient was overweight but previously independent with no comorbidities. After 3 days of constipation, he was given rectally administered fleet enemas. On day 8, the patient developed tachycardia and was febrile to 39.3°. The patient had developed cellulitis over thigh and pubic region, as well as scrotal oedema. He had an escalating white cell count of 18.1 × 109/L to 22.3 × 109/L (reference range 3.7–9.5 × 109/L) and CRP of 52–167 mg/L over 24 hours (normal ≤ 4 mg/L).
In retrospect, the patient reported anal pain during administration of a fleet enema 3 days prior. On inspection of the anus, there was a necrotic area leading into the anal canal. This finding of perianal trauma associated with the increasing evidence of sepsis led to a presumptive diagnosis of FG. CT scan (Fig. 2) demonstrated an area of hazing and small amounts of free gas within the perirectal tissue suggestive of a rectal perforation or FG. The patient was taken to theatre for an urgent intervention. The scrotum and perianal region required debridement of the affected soft tissue (Fig. 1). Sigmoidoscopy demonstrated circumferential necrosis of the lower portion of the rectum consistent with REI (Fig. 3). A decision was made to expectantly manage the rectal injury and perform a repeat sigmoidoscopy with the aim of preserving the rectum in lieu of an urgent rectal resection. The antibiotic regime was changed to meropenem, clindamycin and vancomycin. Tissue cultures from the debridement grew scant colonies of Pseudomonas aeruginosa and Bacteroides uniformis. The repeat sigmoidoscopy demonstrated stabilization of the rectal ischaemia. A diverting colostomy was created to assist in application and management of negative pressure dressings to the perineal wound (Fig. 4). He required 2 days of post-operative ICU support and over the next 2 weeks, symptoms and inflammatory markers returned to normal. An examination under anaesthesia performed 1 week later demonstrated interval improvement of the rectal mucosa with resolving necrosis. The patient was discharged after 3 weeks with no further dressings and the colostomy was reversed 3 months later.
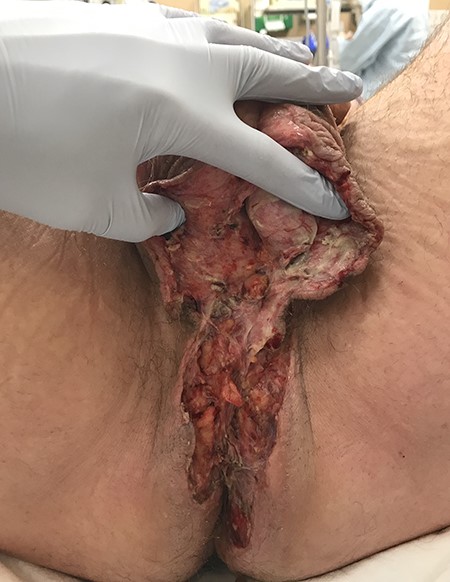
Operative photo. Extent of debrided soft tissue at time of initial intervention.
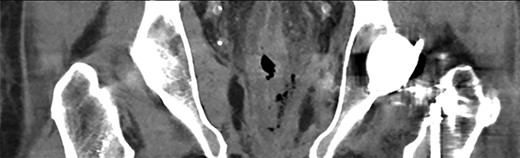
Coronal CT image demonstrating contained, localised rectal perforation secondary to enema injury.
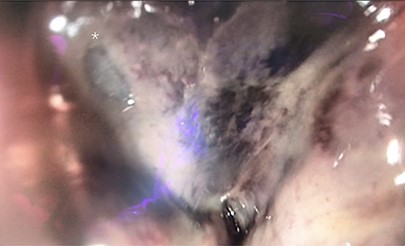
Sigmoidoscopic still of site of rectal injury. Site of perforation marked with Asterix*.

Operative photo. The wound at final operative inspection was partially closed. A negative pressure wound management device was placed to the remaining defect. A diverting colostomy was created in order for the management device to be undisturbed, as the remaining defect was around the anus.
DISCUSSION
The current case highlights a difficult diagnostic dilemma; distinguishing between FG and REI. FG is a fulminant necrotizing fasciitis of the genito-perineal region due to synergistic polymicrobial infection, with a significant association with perianal infection [1]. REI due to perforation caused by a traumatic enema administration results in perianal and rectal chemical-induced inflammation [5]. REI can be classified into five subtypes ranging from anal canal perforations below the level of the levator (grade I) to intraperitoneal perforation (grade V) [6]. The current injury involved a limited retroperitoneal perforation (grade III) and such was managed in an expectant manner.
Expectant management cannot be applied to FG, being a fulminant and potentially life-threatening condition, which requires immediate radical debridement. Diagnosis is initially based on clinical suspicion and often gas in the affected tissue. REI may have a similar clinical and radiological appearance. Diagnostic tools such as the Laboratory Risk Indicator for Necrotising Fasciitis score have limited utility in the diagnosis and prognostication the severity of soft tissue inflammation and infection associated with REI. Diagnosis and management still remains based on clinical suspicion [7]. Imaging such as CT scans, whilst demonstrating the retroperitoneal perforation, do not differentiate between FG and REI. However, the underlying pathophysiology is different, and surgical intervention is more likely to be more conservative debridement and organ preservation. As Pietsch et al. (1977) postulated, pain and ‘pronounced inflammatory response’ is secondary the injection of hypertonic phosphate into tissue rather than mechanical injury [8]. In the setting of FG, a more radical debridement and potential rectal resection would have been required. Judicious interval examinations and flexible sigmoidoscopies allowed for monitoring of the rectal injury and preservation of the rectum.
Colostomy formation in FG remains controversial with no demonstrable prognostic benefit but increased associated cost overall [3]. However, delayed colostomy formation at a ‘second-look’ operation in selected patients is a ‘reasonable’ approach [3]. Faecal diversion and resection of the affected segment is common practice found within the literature for rectal injuries; however, tailored approaches to individual cases are also advocated [9]. In the current case, we successfully debrided all affected tissue and were able to preserve the rectum with judicious monitoring. A diverting colostomy was formed at a secondary debridement in order to divert faeces away from the site of debridement and allow for the effective application of negative pressure wound therapy through the Vac™ system (KCI Acelity, USA). The application of the Vac™ dressing allows for promotion of granulation tissue leading to healing by secondary intention, delayed primary closure or skin grafting [10].
In summary, iatrogenic rectal injury secondary to rectal enema administration is an uncommon but serious complication. However, the initial clinical picture can be misinterpreted as a fulminant FG. This could result in an urgent, radical debridement and resection. The determination of the injury severity through judicious monitoring and effective management of the wound will allow for the preservation of the rectum without resection.
Disclosure
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Reference
Author notes
Author Contributions: All authors contributed equally to the creation and review of the article.



