-
PDF
- Split View
-
Views
-
Cite
Cite
Raju Limbu, Sabrina Brar, Prince Modayil, A case report of an incidental finding of congenital oesophageal diverticulum in a patient presenting with stridor, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa491, https://doi.org/10.1093/jscr/rjaa491
Close - Share Icon Share
Abstract
Congenital oesophageal diverticulum is incredibly rare and has not commonly been published in the literature. Oesophageal diverticulum can be asymptomatic; however, symptoms such as dysphagia, regurgitation and chest discomfort may be present. We describe the case of a paediatric patient presenting with biphasic stridor, respiratory distress and cyanosis at birth, who was found to have a supraglottic cyst and later the presence of an oesophageal diverticulum shown on ultrasound imaging. There has been one other case reported in the literature of an oesophageal diverticulum presenting with stridor, and we therefore believe this is one of only two cases to illustrate this atypical presentation of congenital oesophageal diverticulum. It highlights the importance of a meticulous multidisciplinary team approach to patient care, as well as conducting appropriate investigations to aid early diagnosis to improve patient outcomes.
INTRODUCTION
Oesophageal diverticulum is an acquired protrusion of mucosa and submucosa through a weak part of the muscular layers of the oesophagus. Anatomically, this can occur anywhere along the oesophagus from the throat to the stomach:
pharnygo-oesophageal (posterior/anterior)—this is the most common type of oesophageal diverticulum, known as Zenker’s diverticulum;
mid-thoracic—affecting the middle portion of the oesophagus;
epiphrenic—the inferior oesophagus, superior to the diaphragm [1–4].
Typically, oesophageal diverticulum will present in adults, with male predominance reported [1–4]. If symptomatic, progressive dysphagia and food regurgitation may be noted. Other symptoms and signs include halitosis, chronic cough, gurgling neck sounds, chest discomfort, respiratory distress and aspiration pneumonia [1–3]. The gold standard investigation for diagnosis of oesophageal diverticulum is a barium swallow study, which elucidates the size and location of the defect [4]. If symptomatic or for diverticulum >1 cm, surgery is the main therapeutic approach. There is a trend towards performing transoral endoscopic treatment, a less invasive technique compared with open cricopharyngeal myotomy (with or without diverticulectomy) [5]. Surgery has an excellent prognosis with a 90% success rate reported [1].
This case will be of value to all medical professionals, as it clearly illustrates an unusual presentation of an oesophageal diverticulum in a paediatric patient presenting with stridor. Oesophageal diverticulum should therefore be considered as a differential diagnosis if a similar case presents in the future.
CASE PRESENTATION
A baby was born at term (39 6/7 weeks gestation) after premature rupture of membranes, for which she received 3 days of antibiotics. She initially presented floppy with a low respiratory rate and required supplementary oxygen. Biphasic stridor was audible from birth both at rest and when crying. She presented to the ear, nose and throat (ENT) team at 10 days old with worsening stridor. On examination, she had marked tracheal tug and intercostal recession; cyanotic episodes were noted when feeding and crying with saturations dropping to 80 and 70%, respectively. No vomiting was reported and she was gaining weight appropriately. Flexible nasoendoscopy was performed, which illustrated mild laryngomalacia. Initial management included treatment with steroids and nasogastric feeding.
The patient underwent a computed tomography (CT) scan that illustrated a large left-sided supraglottic cyst (3.5 × 2.4 × 2.9 cm) extending from C3 to C7 with paratracheal extension (Figs 1–3). This was confirmed on microlaryngobronchoscopy (MLB) and the cyst was drained. The patient was managed postoperatively in the paediatric intensive care unit where she remained intubated. Extubation was unsuccessful, secondary to worsening stridor and increased work of breathing; a chest X-ray revealed a collapsed right lung. A second MLB was performed and thick bronchial secretions were found, as well as subglottic inflammation, in keeping with a diagnosis of tracheitis.



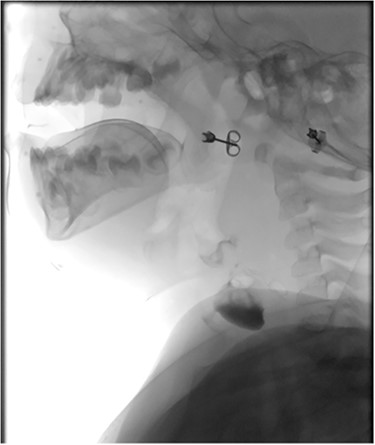
Sagittal barium sallow illustrating the presence of an oesophageal diverticulum, filled with contrast on swallowing.
The patient later underwent a barium swallow and magnetic resonance imaging (MRI), both of which showed a left lower neck cyst with an opening into the left piriform sinus. Differential diagnoses included a foregut duplication cyst or a third branchial cleft anomaly. Ongoing management of the cyst was discussed with a specialist paediatric ENT team who decided to observe the patient, given she was progressing well clinically. Saturations during this time remained >96% during feeding.
At age 8 months, the patient was admitted to hospital from clinic due to worsening stridor. She underwent a further MLB that once again illustrated a cyst. An ultrasound scan was performed intraoperatively to aid with emptying of the cyst, and an incidental finding of a connection between the cyst and the cricopharyngeal region was identified, in keeping with a diagnosis of an oesophageal diverticulum. This was later confirmed on a barium swallow study (Fig. 4). Following the MLB, the patient remained clinically stable; the stridor resolved.
The case has been discussed with the Paediatric, Radiology, and Head and Neck team regarding possible excision of the cyst and management of the oesophageal diverticulum. Ultrasound imaging performed when she was 3 years of age confirmed the presence of a pouch in the cervical oesophagus. The patient is now 4 years old—she has been seen regularly in the ENT clinic and remains clinically well. She continues to be asymptomatic from her oesophageal diverticulum and is therefore being managed conservatively at this time.
DISCUSSION
Cervical oesophageal diverticulum, known as Zenker’s diverticulum, usually manifests in middle-aged/elderly individuals. Predominance in males has been noted. In paediatrics, oesophageal diverticulum is incredibly rare; there has been one previous case report of a paediatric patient presenting with airway compromise that was found to have an oesophageal diverticulum. There are however no reports in the literature of an oesophageal diverticulum presenting in accordance with/as a supraglottic cyst. This paper therefore highlights that although exceedingly rare, oesophageal diverticulum should be considered as a differential diagnosis in paediatric patients presenting with stridor [1–4].
The gold standard imaging modality for investigating the presence of an oesophageal diverticulum is a barium swallow study. In our case, a combination of barium swallow, CT, MRI, ultrasound and direct visualization with MLB was used for diagnosis. With regards to this patient, drainage of her supraglottic cyst alleviated the patient’s airway symptoms, namely stridor; however, definitive treatment such as endoscopic/open surgery may still be required to repair the oesophageal diverticulum, more so if the patient was to become symptomatic. There is little evidence in paediatrics to favour a particular surgical approach to treat oesophageal diverticulum; in adults, there have been no randomized control trials that compare endoscopic versus open surgery [4]. Retrospective reports indicate that smaller (<5 cm) oesophageal diverticulum are best treated endoscopically; however, although general trends are emerging, one cannot draw firm conclusions between the suitability and superiority of the various treatment options currently available. Furthermore, the transferability of such data from adults to children may not be conclusive.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



