-
PDF
- Split View
-
Views
-
Cite
Cite
Roberto Cunha, Rafaela Parreira, Rui Quintanilha, Vítor Carneiro, Armando Medeiros, Inês Leite, Heterotopic gastric mucosa in the gallbladder—a rare find, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa490, https://doi.org/10.1093/jscr/rjaa490
Close - Share Icon Share
Abstract
It is universally known and accepted that the development of a certain type of tissue outside its usual location, like in the gastrointestinal tract, can occur. This is a relatively common situation in the upper region of the gastrointestinal tract. However, the development of gastric mucosa in the gallbladder is a rare find. The following is the case of a 22-year-old male with an 18 mm gallbladder polyp, who electively underwent a laparoscopic cholecystectomy, having been diagnosed at a histopathological level with heterotopic gastric mucosa in the gallbladder. This brief article also aims to provide a reflection on the possible evolution of neoplasms from this histological change, based on the doubts raised in literature.
INTRODUCTION
Heterotopic or ectopic tissue is defined as the presence of tissue outside its normal location, devoid of neural, vascular or anatomic connection to the main body of an organ in which it normally exists [1]. Heterotopic gastric mucosa is most often located in the upper gastrointestinal tract [2]. However, it can appear throughout the whole gastrointestinal tract as it is known, for example, in Meckel’s diverticulum [3]. The development of gastric mucosa in the gallbladder is a rare find, with ~34 cases reported in the existing literature. Other tissues such as liver, adrenal and thyroid have already been described in the gallbladder [1]. As heterotopic tissue may promote carcinogenesis of the gallbladder, close attention should be paid to any occurrence of such lesions in this anatomical region.
CASE REPORT
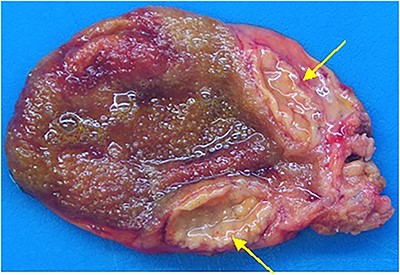
A 22-year-old male with smoking habits was periodically followed in internal medicine consultations for epigastric abdominal pain, in which, through endoscopic examinations, a Helicobacter pylori positive test was identified. Once the eradication of H. pylori was completed and confirmed, the patient started experiencing symptoms of recurrent pain in the right hypochondrium. His blood tests were normal. An abdominal ultrasound was performed, which revealed a nodular image adhering to the internal wall (not moving with positional changes) with 18 mm, found in the infundibular region. It was echogenic with an anechoic center. These aspects were compatible with sessile polyp with a necrotic center associated with surrounding parietal thickening. In order to obtain further clarification, an endoscopic ultrasonography was carried out, which confirmed a homogeneous echogenic lesion with central hypoechogenicity with a larger transversal diameter of 18 mm adhering to the wall (Fig. 1). In this context, the patient was proposed for elective laparoscopic cholecystectomy, which occurred without complications. After surgery, microscopy revealed a cavitated polyp consisting largely of gastric body mucosa, although pyloric type mucosa was still found, with no intestinal metaplasia or epithelial dysplasia being identified (Fig. 2—macroscopic examination/Fig. 3—microscopy).
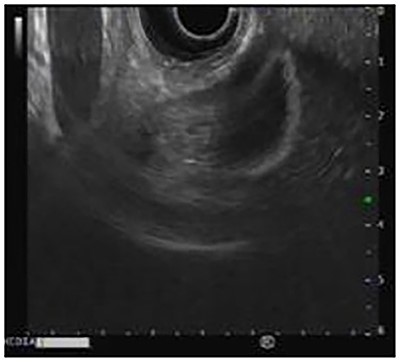
Endoscopic ultrasound shows an echogenic polyp in the infundibulum of the gallbladder.
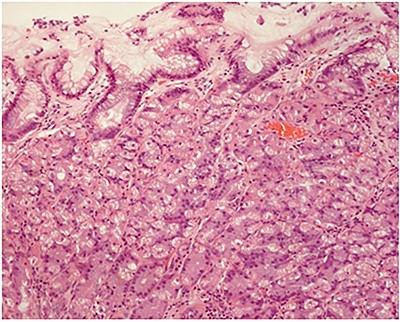
Fundic (oxyntic) gastric gland mucosa (hematoxylin and eosin; ×100).
DISCUSSION
In a systematic review on this subject, it is described that this change is found equally in males and females, with an average age of 36.4 years [3]. Clinically, heterotopic gastric mucosa manifests symptoms such as colicky pain in the epigastric or right hypochondrium, associated with nausea and vomiting [1], although sometimes it can also be described as asymptomatic or even an accidental finding [4]. About 50% of patients had normal blood examination; however, sometimes they had elevated transaminases and gamma-glutamyltransferase or leukocytosis caused by disturbed bile flow leading to inflammatory reactions. In the ultrasound diagnosis, a polypoid mass of broad or sessile base, usually hyperechoic, was found. Regarding the localization, the cystic duct and the gallbladder neck were the most frequent sites [3].
Heterotopic gastric mucosa in the gallbladder is a rare condition that raises many doubts regarding the causes of its development and the consequences thereof. There are some proposed causes for the appearance of heterotopic gastric mucosa, such as the entrapment of primitive gastric tissue [6], abnormal development, heterotopic differentiation or the metaplastic differentiation [1]. However, due to absence of a clear embryological explanation and the extreme rarity of the condition, the etiology of this situation remains unknown. Regarding the consequences, Ishii et al. [7] suggested that heterotopic gastric mucosa may have the potential for carcinogenesis. Although no malignant transformation has yet been reported, dysplasia in heterotopic gastric mucosa in the gallbladder has been already reported [7]. Thus, it is considered that carcinoma must be ruled out in polypoidal lesions of the gallbladder >1.0 cm due to the high incidence of gallbladder carcinoma in sessile polypoidal lesion [8]. Another possible consequence of the existence of gastric tissue in the gallbladder is ulceration [1].
Thus, considering that preoperative diagnosis is impossible, it is necessary to use imaging characteristics to establish a differential diagnosis between benign and malignant polyps. Benign polyps are usually <10 mm in size, whereas carcinoma or heterotopic gastric mucosa may have larger dimensions [9]. If a computed tomography is performed, one difference is the hypovascularization of the carcinoma in contrast to the hypervascularization of the heterotopic gastric mucosa [10]. Another way in which it can be differentiated is based on the location, as the heterotopic gastric mucosa is usually located in the neck of the gallbladder and the carcinoma can infiltrate the gallbladder fossa.
In conclusion, once the final diagnosis is made by histopathology, it is the surgeons’ role to look into an eventual heterotopic gastric mucosa in young patients with symptoms of cholecystitis or cholelithiasis and gallbladder polyps, while not being neglectful of the differential diagnosis of a possible carcinoma. It is worth remembering that despite the cause that underlies the symptoms, cholecystectomy is always the indicated intervention for large polyps and symptomatic patients.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that his name and initials will not be published, and due efforts will be made to conceal his identity.
CONFLICT OF INTEREST
None declared.
FUNDING
None.
References
Uchiyama, S., Imai, S., Suzuki, T. et al.



