-
PDF
- Split View
-
Views
-
Cite
Cite
Hazim Hakmi, Hassan Hashmi, Jackson Hunt, Jun Levine, Laparoscopic repair of incarcerated transverse colon internal hernia in a patient with Crohn’s disease, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa482, https://doi.org/10.1093/jscr/rjaa482
Close - Share Icon Share
Abstract
Internal hernia is a rare cause of bowel obstruction in patients with no prior surgical history. Laparoscopic repair of a transverse bowel herniation through the foramen of Winslow is the rarest type of internal hernia, with only two case reports published in the literature. In a patient with a history with Crohn’s disease and no prior surgical history, presenting with signs of bowel obstruction, and no inflammatory symptoms, internal hernia should be suspected as one of the causes. Minimally invasive laparoscopic repair is a feasible safe option in those patients, allowing patients to go home the next day postoperatively.
INTRODUCTION
Abdominal hernias account for a significant number of bowel obstructions (BO), with internal hernias in patients with no prior surgical history being a rare subcategory causing BO. Foramen of Winslow (FOW) is one of the rare internal hernia defects that could lead to BO, with transverse colon being the rarest form of bowel to herniate through it. We present this rare incidence in a patient with Crohn’s disease as the underlying condition that could have led to enlargement of the foramina defect, keeping in mind that abdominal pain, obstipation in a patient with Crohn’s disease and no prior surgical history could be due to an internal hernia, not an inflammatory flare up.
CASE REPORT
An 80-year-old female with past medical history of Crohn’s disease (diagnosed in 1998 and managed with Adalimumab) and no prior abdominal surgical history who presented with 1-day history of severe epigastric pain associated with nausea and emesis. Her last colonoscopy was 3 years ago (unremarkable), and last Crohn’s flare was a 1 year beforehand. On examination, patient’s abdomen was soft with severe epigastric tenderness and an appreciable bulge. Labs showed normal lactate (1.1) but mild leukocytosis of 12.5 and no other gross lab abnormalities. Patient underwent computed tomography (CT) scan of abdomen and pelvis which showed a transverse colon herniating through the FOW and causing a closed-loop obstruction (Figs. 1–3). Patient was immediately decompressed with a nasogastric tube and was emergently taken to the operating room for a diagnostic laparoscopy. Intraoperatively, the transverse colon was noted to have herniated through the FOW into the lesser sac. The incarcerated transverse colon appeared immensely dilated and hyperemic. With careful traction and gentle counter pressure, the transverse colon was completely reduced from the FOW back into the abdominal cavity. On inspection after reduction, the small and large bowel appeared grossly viable and well-vascularized along with adequate peristalsis. The FOW was closed with 2-0 ethibond running suture by suturing the peritoneum adjacent to the portal triad down to the retroperitoneum just lateral to the inferior vena cava. The patient tolerated the procedure very well and brought to the recovery room in stable condition. Postoperatively, the patient did very well. On postoperative Day 1, the patient was discharged home. Subsequently, the patient was seen in the office on postoperative follow-up Day 7 and was found to be doing well with no complaints.
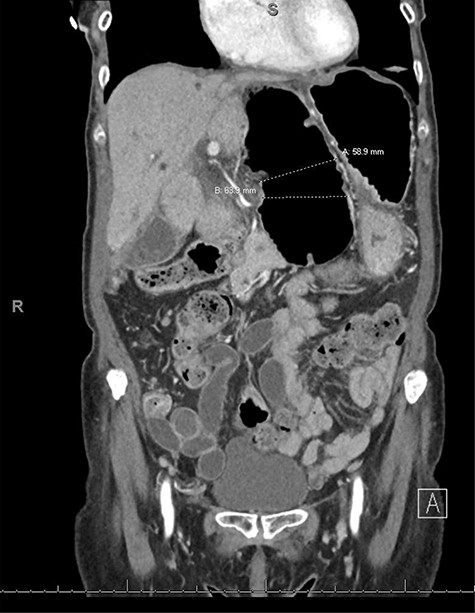
CT coronal view showing dilated loop of transverse colon medial to the lesser curvature of the stomach dilated to ~6 cm, which is involved in an internal hernia.

CT coronal view showing proximal and distal loops of transverse colon are seen in the region of the foramen of Winslow.
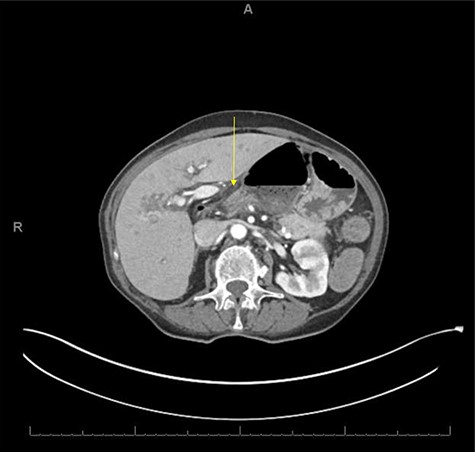
CT axial view showing proximal and distal loops of transverse colon are seen traversing through the foramen of Winslow.
DISCUSSION
BO is commonly reported in patients with inflammatory bowel disease (IBD), with internal hernias causing BOs in that subpopulation due to prior surgeries, but rarely if ever do patients with IBD present with BO due to internal hernias in patients those with no surgical history.
Internal hernia is a protrusion of the abdominal viscous through either a constitutional defect, or an acquired defect that was created by prior abdominal surgical intervention, trauma or inflammatory processes. Internal hernia is estimated to be 2% of all causes of internal obstruction Preoperative diagnosis of internal hernias can be difficult sometimes due to the nonspecific clinical presentation, but with CT, the diagnosis process has been easier.
Internal hernias can be classified into six major groups. Paraduodenal hernias being the most common, FOW hernias, transmesenteric hernias, pericecal hernias, intersigmoid hernias and paravesical hernias. The incidence of congenital/constitutional internal hernias is much lower than acquired internal hernias. Frequency of FOW congenital internal hernia BO is 8% in comparison to other congenital internal hernias [1].
IBD flare-ups causing a BO can be managed initially nonoperatively, but closed-loop obstructions due to internal hernias are surgical emergencies that need to be emergently taken to the operating room. It is unclear if the inflammatory state cause by IBD can lead to mesenteric redundancy that could be a risk factor for developing large defects and loose transverse colon attachments, allowing the transverse colon to herniate through the FOW.
BO due to adhesions can sometimes be managed initially nonoperatively in stable patients for a few days awaiting spontaneous resolution. IBD BO can also be managed initially nonoperatively in stable patients with steroids and anti-inflammatory medications, hoping that will help relieve the obstruction. Although internal hernias have to be surgically explored and reduced operatively with no room for conservative management, due to the high risk of bowel ischemia [2]. Although spontaneous reduction of the hernia may occur.
In a literature review by Moris et al. looking at laparoscopically repaired internal hernias of FOW with bowel reduction, they found that the most frequent viscera herniating through the FOW was the ileum, followed by the cecum [2]. Right/ascending colon herniation was seen in three cases, whereas transverse colon herniation was seen only in two case reports. They also noticed that there has been an increased tendency to surgically reduce BO due to internal hernias via laparoscopic approach [3, 4]. Laparoscopic surgery allows for shorter length of stay, a more rapid recovery and lower pain scores except in patients undergoing mesh placement as described by Velanovich [5].
Regarding the technical aspects of the procedure, usually four trocars are placed, one supraumbilical (or infraumbilical) and another three 5-mm ports in the left and right lumbar regions as well as the epigastrium. Rarely is bowel decompression needed. Gallbladder puncture might be necessary in some cases to reduce a highly tense gallbladder hernia. The closure of the FOW defect is contreversial (whether with sutures or ommentopexy), as no internal hernia recurrence has been reported after bowel reduction.
In conclusion, surgeons should have internal hernia of the large or small bowel in their differential when patients with IBD present with symptoms of BO, albeit a rare pathology to happen. Computer tomography is the standard diagnostic choice for imaging. As surgeons are more comfortable with laparoscopic techniques, laparoscopic treatment is a safe surgical option in those patients.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



