-
PDF
- Split View
-
Views
-
Cite
Cite
Josiah Damisa, Zereda Zulkeefli, Lebur Rohman, David Burton, Shoulder septic arthritis following routine influenza vaccination, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa458, https://doi.org/10.1093/jscr/rjaa458
Close - Share Icon Share
Abstract
The UK vaccination guidelines state that skin cleansing is not essential in socially clean patients. This report discusses a 69-year-old type 2 diabetic patient with a 4-week history of left shoulder pain with no precipitating factors other than a ‘flu vaccination without having had skin alcohol cleansing. She sustained a swollen left painful shoulder. Aspiration fluid grew Staphylococcus aureus and imaging confirmed diagnosis of septic arthritis. She underwent shoulder debridement and was started on antibiotics. Imaging 6 months later shows the sequelae of septic arthritis. The patient had ongoing stiffness and pain at 6 months. This report raises the question of whether there needs to be a revision of routine skin cleansing practice before vaccinations in certain groups of individuals.
INTRODUCTION
Septic arthritis may be caused by haematogenous spread, direct inoculation or as a complication of surgery. The joints most commonly affected are knee and hip [1].

X-ray imaging showed degenerative changes in the glenohumeral and acromioclavicular articulations.

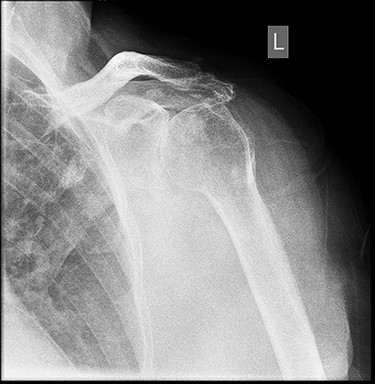
Six months post-surgery—profound loss of joint space and superior subluxation.
We report a specific route of inoculation through vaccination. Seasonal influenza vaccination is provided to vulnerable groups of people who are at an increased risk of complications to influenza virus. These groups of people include people with immunosuppressive disease and chronic illness. It is also provided to certain individuals who have access to vulnerable groups in long-stay residential facilities such as prison, hospitals, halls of residence and healthcare workers [2].
CASE REPORT
A 69-year-old female presented with a 4-week history of left shoulder pain with no other precipitating incident other than a flu vaccination weeks earlier on the left shoulder, with clinical notes indicating no routine disinfection was carried out prior to injection.
Past medical history includes hypertension, AF (on warfarin) and Type 2 diabetes mellitus (T2DM) on Metformin.
On examination, she presented with a swollen left shoulder with no movement due to pain; there was no distal neurovascular deficit. Blood tests revealed elevated inflammatory markers with a CRP of 149 mg/L and ESR of 134 mm/h and minimally raised white cell count (WCC) of 11.1 × 109/L. Aspirated fluid grew Staphylococcus aureus (SA) on culture.
Clinical observations were at baseline levels with a temperature of 36.1°C, pulse of 70 bpm and BP of 125/67.
X-ray imaging showed degenerative changes in the glenohumeral and acromioclavicular articulations with inferior displacement of the humeral head.
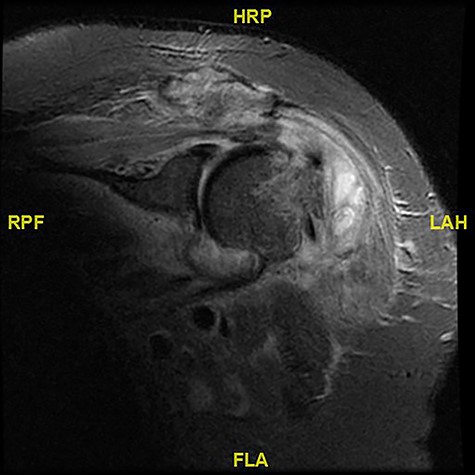
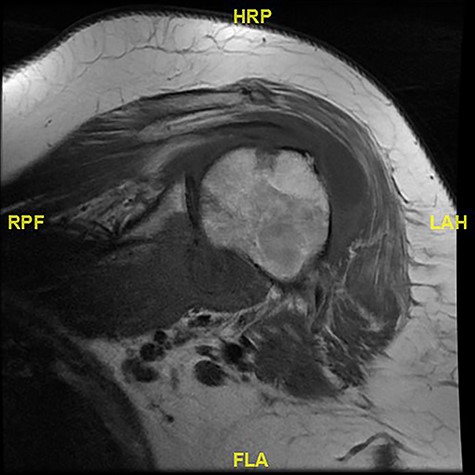
Magnetic resonance imaging (MRI) showed walled off loculations of pus around the proximal humerus with myositis and evidence of septic arthritis.
She underwent left shoulder open debridement and was started on flucloxacillin. Five months later, there was a reduction in serum markers with CRP 16 g/L, ESR 55 mm/h and WCC 7.4 × 109/L. She received weekly physiotherapy to increase her range of movement (ROM).
X-ray images 6 months later showed the devastating effect of the infection with a profound loss of joint space and superior subluxation in keeping with loss of rotator cuff muscles.
Shoulder examination 10 months later showed a forward flexion of 50°, abduction of 40° glenohumeral through to 70° with scapulothoracic movement, internal rotation to buttock and external rotation of 20°. Although there was improved ROM, she still struggled with extremes of movements such as brushing her hair and this was attributed to the presence of underlying arthritic changes of the shoulder caused by the infection.
DISCUSSION
Injected flu vaccinations are commonly administered via IM route. Several studies indicate that skin cleansing is not a requirement for vaccination and in the rare occasion where the skin looks visibly dirty, cleansing can be achieved with soap and water, however skin cleansing with alcohol has been controversial in clinical settings [3, 4].
The commonly held practice was to cleanse the skin with alcohol before vaccination; however, a vaccination memorandum by the Ministry of Health in 1962 acknowledged that many doctors did not use alcohol. This began a change which led to the current norm of no skin cleansing before vaccination [5]. Should there then, as evident in the case report, be any need for a revision of routine skin cleansing practice before vaccination in some groups?
Alcohol has shown a reduction of 82 to 91% in microbial population on the skin surface when applied for 5 s. Despite this reduction, another study revealed that following prolonged disinfection for 5 min, 20% of sub-epidermal bacteria were still present post-disinfection and on some surfaces, such as the scalp, ~50% of bacterial population were still present post-disinfection [6].
Therefore, it could be argued that sub-epidermal bacteria remnants could still be sources of infection when insertion of needle further pushes the bacteria deeper into the body tissues. To determine the critical amount of bacterial population required to cause an infection, a study showed the minimum concentration of SA required for infection to occur via intradermal inoculation is 1 million cocci per 0.1 ml, a bacteria concentration not present in the nasal droplet of 100 microns diameter despite the nasal cavity being one of the natural habitats of SA in humans. However, this study failed to show if the minimum concentration in an immunocompromised patient would be much lower [7].
Public Health England have stated that despite alcohol reducing the bacterial count on the skin, it does not eliminate the bacteria beyond the reach of the wipes, the ones under the skin surface in ducts, glands and follicles and hence still carries the same risk of infection. This is important as 10-fold times more bacteria are found under the skin than the ones on the surface (typically about 1000/cm2) and hence only a minimal reduction is achieved by alcohol cleansing [5].
A prospective study comparing the effects of pre-venesection skin cleansing to no skin cleansing showed no statistically significant difference in the two groups with respect to complications at the venesection site on day 1, 3 and 5 [8].
The UK vaccination guidelines state that skin cleansing is not essential in socially clean patients, although soap and water can be used when the practitioner feels the skin needs to be cleaned. WHO’s guidelines however recommend the use of soap and water before vaccination but discourages the use of alcohol [4, 5].
However, the Public Health Laboratory Service states that despite the continual use of alcohol cleansing, it is only useful to remove or kill transient organisms, not the common causative organism in wound infection or septic arthritis [5].
The patient’s coexisting medical conditions; warfarin treatment for AF and T2DM could however be confounding factors. A common complication of T2DM is the increased risk of infection [9].
A retrospective study carried out on 647 patients, evaluating haematoma and abscess after neuraxial anaesthesia, suggested that patients on warfarin who underwent epidural anaesthesia and subsequently developed hematoma could be predisposed to an increased risk of an abscess as there is an increase in bacterial colonization at the insertion point 48 h following skin insertion [10].
In conclusion, this report highlights a potential subgroup of vaccination subjects who are being offered influenza vaccination by virtue of perceived increased risk of contracting flu or at greater risk of complications of flu. This is by virtue of their general health and immune status.
This patient suffered and continues to suffer a significant complication secondary to vaccination into the deltoid. This raises the question as to whether a greater level of care with skin disinfection is required in this subgroup.
Notwithstanding these caveats, it of course behoves the practitioner to maintain sterility when preparing the syringe and needle during a procedure.
ACKNOWLEDGEMENTS
We would like to acknowledge the patient who this case study is based on.
CONFLICT OF INTEREST STATEMENT
None declared.
References
Influenza [PHE, 2018] and Contraindications and special considerations [PHE, 2018] in the Public Health England document Immunisation against infectious disease. In:



