-
PDF
- Split View
-
Views
-
Cite
Cite
Genevieve Hattingh, Ruben D Salas-Parra, Afrin Nuzhad, Joselyn Salvador, Daniel T Farkas, Duodenal perforation in the pediatric population: two rare cases at a small community hospital, Journal of Surgical Case Reports, Volume 2020, Issue 11, November 2020, rjaa455, https://doi.org/10.1093/jscr/rjaa455
Close - Share Icon Share
Abstract
Duodenal ulcer perforation is very uncommon in the pediatric population; hence, it is usually not considered in the differential diagnosis of acute abdomen in this age group. In our small community hospital, we had two rare cases of perforated peptic ulcer in the pediatric population within a short span of time. A 14-year-old male and a 13-year-old female child presented to the emergency room with acute abdominal pain. No other symptoms were reported and neither had any history of peptic ulcer disease. Abdominal CT showed pneumoperitoneum consistent with perforated hollow viscus. Subsequent exploratory laparotomy indicated perforated duodenal ulcer in both children. These cases illustrate that perforated peptic ulcers should be considered in children presenting with acute abdomen.
INTRODUCTION
Peptic ulcer disease (PUD) is uncommon in the pediatric population [1]. The prevalence of peptic ulceration was 8.1% in children undergoing upper gastrointestinal endoscopy for abdominal pain, the majority being males in their second decade of life [2]. As a result of how uncommon it is, its diagnosis is usually not considered unless it presents with perforation or hemorrhage. The main risk factors in the pediatric age have been identified as Helicobacter pylori infection and non-steroidal anti-inflammatory drug ingestion [3].
CASE SERIES
Case 1: A 14-year-old boy with a 2-day history of mild abdominal pain presented to the emergency department (ED) within 6 hours of sudden-onset severe abdominal pain, persistent, mostly in the periumbilical area. He denied nausea, vomiting, diarrhea, fever, melena and hematochezia. Past medical history only significant for ADHD on Adderall. On exam, he appeared in severe distress, with normal vital signs, diffuse abdominal rebound tenderness and rigidity. Laboratories revealed elevated white blood cell count (WBC) of 14.900/L and normal C-reactive protein. Abdominal ultrasound was unremarkable, but since the concern for acute abdomen, a computer tomography (CT) of the abdomen and pelvis was obtained, demonstrating a large pneumoperitoneum predominantly in the upper abdomen suggestive of perforated viscus (Fig. 1).
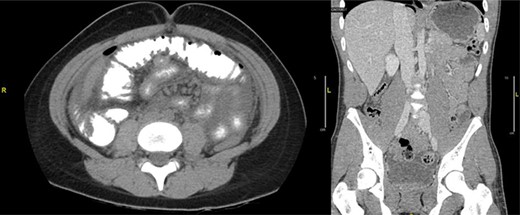
(a) CT abdomen and pelvis axial view. (b) CT abdomen and pelvis coronal view: there is a large pneumoperitoneum predominantly in the upper abdomen.
The patient was taken to the operating room for diagnostic laparoscopy. A 4-mm perforated duodenal ulcer by the pylorus with leaking bile was found and repaired with an omental patch. On postoperative Day (POD) 3, an upper gastrointestinal study was done, which showed no signs of obstruction or leak (Fig. 2). Serum gastrin levels were reported normal. On POD 4, he was started on a diet. He tested positive for Helicobacter pylori and was therefore treated with eradication triple therapy (proton pump inhibitor, amoxicillin and clarithromycin). The patient recovered uneventfully and was discharged home on POD 7, and was symptoms free at follow-up.

Upper gastrointestinal series (a)/small bowel follow-through (b): normal stomach demonstrated. Normal duodenum and proximal jejunal loops. No contrast extravasation identified. Oral contrast in the distribution of stomach, duodenum and proximal jejunal loops with no evidence for extravasation.
Case 2: A 13-year-old girl presented to the ED with a 3-day history of severe diffuse intermittent abdominal pain, worse in the periumbilical area, associated with nausea, vomiting and non-bloody diarrhea. No significant history was reported. On exam, the patient appeared sick, in acute distress, tachycardic and tachypneic with abdominal exam revealing diffuse tenderness with peritoneal signs. Laboratories showed normal WBC but lactic acidosis. Chest X-ray did not show free air under diaphragm (Fig. 3) and abdominal ultrasound showed moderate fluid in right upper quadrant of abdomen, for which CT of the abdomen and pelvis was ordered and it revealed free mesenteric fluid and extraluminal air in the pelvis suspicious for hollow viscus perforation (Fig. 4).
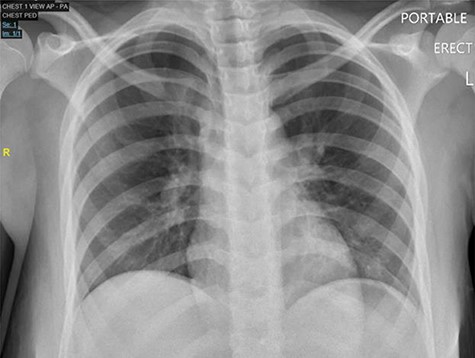
Chest X-ray PA, showing no cardiopulmonary disease, or free air under diaphragm.

Diffuse infiltration of the mesentery is seen. A component of bowel wall thickening is seen in the distal ileum and the transverse colon. In the pelvis, a focus of extraluminal air is seen on the right. Free mesenteric fluid is seen as well.
The patient was taken to the operating room for diagnostic laparoscopy and ~2 L of pus and bile stained fluids were drained. A large anterior perforated duodenal ulcer measuring 2 cm × 1 cm was found. We converted to an exploratory laparotomy and closed the perforation with 3–0 silk sutures. An esophagogastroduodenoscopy was performed intraoperative showing an additional giant ulcer with necrotic slough on the superior and posterior aspect of the first part of the duodenum, for which then we decided to perform a gastroduodenostomy [WU3] and paraduodenal drain placement. She had a prolonged hospital course complicated by enterocutaneous fistula, acute respiratory distress syndrome, pneumonia and acute tubular necrosis for which she remained intubated until POD 26. The patient was discharged home on POD 40. H. pylori was negative. At follow-up, the patient was recovering well without any complications.
DISCUSSION
Differential diagnosis of acute abdomen in children should include perforated peptic ulcers (PPU) as our cases illustrated. PPU is uncommon in children but should be considered in order to avoid a delay in diagnosis and subsequent operative management. Such delay increases likelihood of postoperative complications as seen in our second case [4]. Risk factors such as delay in surgery greater than 12 hours, female gender, age and large perforations increase mortality [5]. Duodenal ulcers are more common than gastric ulcers in children, with an 18:4 ratio [5]. Perforation in children has an occurrence of 0–9% in PUD with duodenal ulcers and is seen more frequently in those older than 7 years [6]. In a large study, the mean age for pediatric PPU was 14.2 years, with 90% being adolescents, also most patients in the pediatric age group presented at the time of perforation which were also similar to both of our cases [5].
Radiography is important in pediatric patients presenting acutely as they present with pneumoperitoneum [6], but studies have shown that X-ray may provide no radiological evidence of perforation as was seen in our case [WU4] [7]. CT reliably detected pneumoperitoneum in our cases. Thus, CT is valuable in the rapid diagnosis of PPU as it allows for prompt treatment and contributes to successful outcomes.
In our first case, PUD was secondary to H. pylori. A retrospective study of 20 years reviewing 52 children who were diagnosed with PUD in their hospital, 7.7% had H. pylori infection. In another study, only 15% of patients with PPU were confirmed to have H. pylori [7]. Other potential causes of perforations have been found to be NSAIDs, trauma and chronic steroid administration [5], but the underlying etiology of our second case is unclear.
In those who present with recurrent abdominal pain with signs or symptoms of PUD, endoscopic management may be appropriate as well as proper definitive therapy to prevent future complications [8]. For those, testing positive for H. pylori adequate treatment should be provided in the form of triple therapy [8].
CONCLUSION
Both of these cases demonstrate that even though PPU is extremely rare in the pediatric population, it must be suspected in children who present with acute abdominal pain and peritoneal signs, as PPU is a surgical emergency and is associated with up to 30% mortality [9]. Early diagnosis is essential to a timely treatment and lower morbidity. Since X-rays may be unremarkable, CT imaging should be considered in children presenting with acute abdomen.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



