-
PDF
- Split View
-
Views
-
Cite
Cite
Ming-Chi Kuo, Jui-Chang Tsai, Fon-Yih Tsuang, Endoscopic discectomy and debridement for a patient with spondylodiscitis caused by Granulicatella adiacens following mitral valve repair: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 11, November 2020, rjaa407, https://doi.org/10.1093/jscr/rjaa407
Close - Share Icon Share
Abstract
We present the case of 40-year-old female patient had severe low back pain after robotic mitral valve repair for chordae tendineae rupture of anterior mitral leaflet. Lumbar-spine magnetic resonance imaging and blood culture diagnosed with Granulicatella adiacens spondylodiscitis at L5-S1, which was successfully treated with percutaneous spine endoscopic debridement and prolonged antimicrobial treatment. Early isolation and treatment of pathogens may decrease the need for surgical intervention with rapid recovery and a shorter duration of hospitalization. We should be aware of the diagnosis of spondylodiscitis when a patient has low back pain with a previous cardiac or dental procedure history. Endoscopic discectomy with debridement is a minimally invasive, safe, direct visualization and effective approach for treatment of infectious spondylodiscitis and is beneficial for symptom relief.
INTRODUCTION
Spondylodiscitis occur at a rate of 2–7% of all musculoskeletal infections [1]. It is characterized by marked heterogeneity, which limits its scientific evaluation and has resulted in a lack of recommendations for treatment [2]. Spondylodiscitis is usually a monobacterial infection and >50% of cases in Europe are caused by Staphylococcus aureus, followed by gram-negative pathogens such as Escherichia coli (11–25%) and Mycobacterium tuberculosis [2].
Granulicatella adiacens is a gram-positive streptococci that is a normal constituent of the human oropharyngeal, gastrointestinal and urogenital flora [3]. Granulicatella adiacens has been involved in cases of bacterial endocarditis and bacteremia and has also been associated with other invasive infections, including abscesses and meningitis [4, 5].
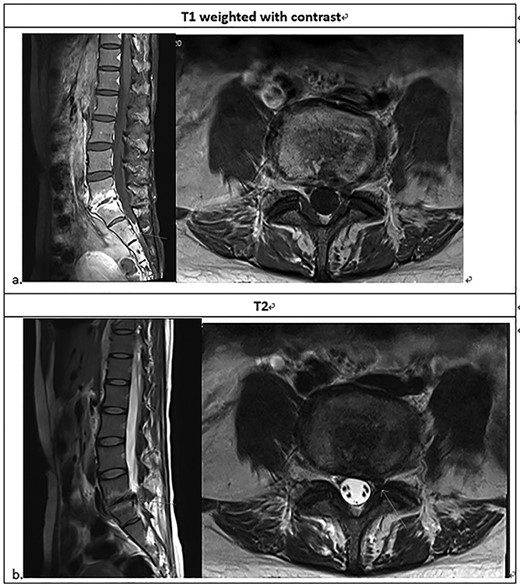
Lumbarsacral spine MRI (a) posterior bulging disc at L5-S1; extruding disc at the left subarticular zone of the left L5-S1, with compression of the left S1 nerve root; neural foraminal stenosis at left L5-S1; increased enhancement at L5-S1 related to the spondylitis change; (b) The arrow point at neural foraminal stenosis at left L5-S1.
Surgical intervention for spondylodiscitis comprises a multidisciplinary approach that includes antibiotics, open/percutaneous biopsy and open/minimally invasive debridement surgery.
Here, we present a rare case where 1 month after mitral valve repair for chordae tendineae rupture, a 40-year-old woman was diagnosed with spondylodiscitis at L5/S1 by an unusual microorganism, Granulicatella adiacens.
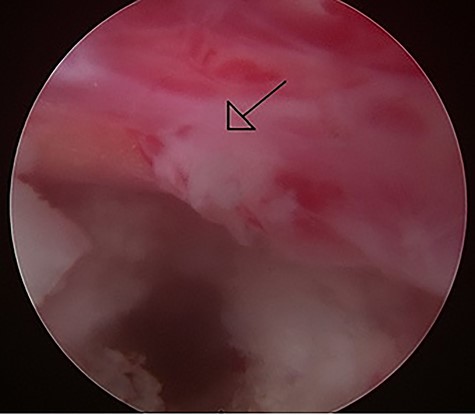
Intraoperative image of the percutaneous endoscopic interlaminar lumbar discectomy at the L5/S1 level left S1 root with hyperemic inflammation was noted after the protruding disc was removed.
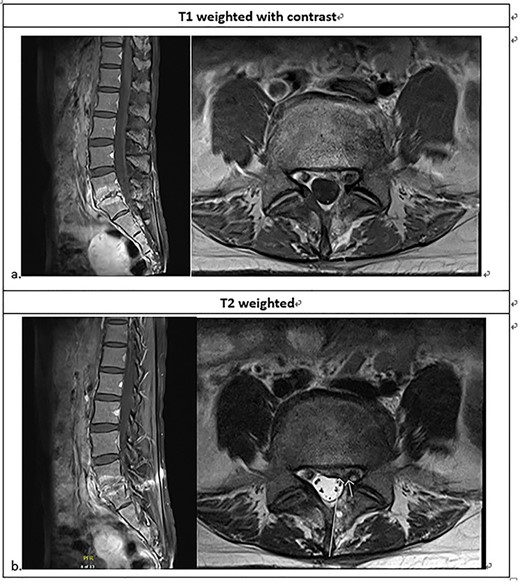
Lumbosacral MRI ~3 weeks after the intervention; less enhancement compared to the previous MRI at the L5-S1 intervertebral disc with adjacent endplates, consistent with spondylodiscitis; less compression of the left S1 nerve root.
CASE REPORT
A 40-year-old woman had a history of low back pain with onset when the patient was 20 years old. Magnetic resonance imaging (MRI) showed degenerative disc disease at L5/S1 only, and her low back pain then resolved after conservative treatment with rest and oral analgesics.
Due to chordae tendineae rupture of anterior mitral leaflet with moderate mitral regurgitation, she received robotic mitral valve repair (28 mm Cosgrove-Edward band, artificial chordae between A3-posteriolateral papillary muscle) in December 2018. The cardiac echocardiogram showed no vegetation on cardiac valve before and after the surgery. She had to take warfarin and was confined to a significant amount of bed rest. However, 3 weeks after the valvuloplasty, she started to notice progressive low back pain. Her low back pain was aggravated by movement, weight loading and alleviated by lying flat. Left sciatica also developed after 1 month of rest.
She was referred to our institute for spine consultation at 3 months after surgery. On physical examination, she had numbness at the left S1 dermatome and saddle anesthesia. Visual analog scale was 8 when admission. The straight leg raising test was bilaterally negative. She had no lower extremity weakness. Contrast-enhanced lumbar-spine MRI showed posterior bulging disc with decreased disc space and endplate changes of L5-S1. We suspected an extruding disc in the left subarticular zone at left L5-S1, compressing the left S1 nerve root. There was increased enhancement at L5-S1, but the paraspinal soft tissue was clear without enhancement (Fig. 1).
Laboratory data showed no leukocytosis (WBC: 7.65 k/μl), platelet: 337 k/μl, C-reactive protein (CRP): 3.33 mg/dl, and erythrocyte sedimentation rate: 39 mm/h, which suggested inflammation. Her blood culture was repeatedly found to be positive for Granulicatella adiacens (time to positive time: 5.95 h). Transthoracic echocardiography showed prior mitral valvuloplasty with moderate mitral regurgitation. No vegetation was noted. Mild pulmonary hypertension was also noted (max TR PG = 31 mm Hg).
After admission, vancomycin was given based on blood culture report. Her low back pain persisted. Thus, percutaneous endoscopic interlaminar lumbar discectomy to the left of L5/S1 was performed 5 days later.
During the operation, a bulging fragile disc with purulent debris was noted. After removal of the disc, the left S1 nerve root expanded well (Fig. 2). No obvious purulent fluid accumulation was noted. After the surgery, her left sciatica and low back pain improved. Her CRP also decreased to 0.69 mg/dl, and repeated blood cultures were negative for pathogens. Her intraoperative specimens did not reveal any pathogens on bacterial culture. Antibiotics with intravenous vancomycin had been given for 14 days and were shifted to oral amoxicillin upon discharge.
Follow-up MRI after 1 month of antibiotics showed little change at the L5-S1 intervertebral disc and adjacent endplates, consistent with partially treated spondylodiscitis. There was also less compression of the left S1 nerve root (Fig. 3).
DISCUSSION
Spondylodiscitis can occur as a primary infection of the intervertebral disk or secondary to blood-borne spread. Predisposing factors to spondylodiscitis include surgical and dental procedures, intravenous drug abuse, elderly age, immunocompromise, malignancy and chronic steroid usage [2]. Symptoms such as fever or leukocytosis may not be present. However, the presence of elevated inflammatory parameters, such as high erythrocyte sedimentation rate and CRP, are much more consistent.
Granulicatella adiacens have stronger degree of infectivity, and this has been attributed to its capacity to bind to the cardiac valvular tissue [4]. The most common valves affected are the aortic and the mitral valves with detectable vegetations being observed in ~64% of cases [6]. Only a few cases with spinal infection have been previously reported, especially in regards to spondylodiscitis after valve surgery.
Granulicatella are sensitive to clindamycin and vancomycin [4]. For cases with infective endocarditis due to Granulicatella adiacens, combination therapy with penicillin and aminoglycoside is recommended. In spite of good in vitro results, treatment failure is observed in 41% of cases, and 27% require prosthetic valve replacement, especially since congestive heart failure or major systemic emboli, relapse and death are also common, affecting 17–27% of patients [4].
Surgical intervention is usually reserved for patients who do not respond to antibiotic therapy, or patients with spinal deformity, instability, epidural abscess or neurologic deficits. Endoscopic surgery is a minimally invasive, simple and safe procedure that provides real-time images with direct visualization and an effective approach for treatment of infectious spondylodiscitis and is beneficial for symptom relief. Endoscopic surgery can also obtain enough sample directly from the infected area for culture. Epidural or paravertebral abscesses initiating from the anterior spinal column can also be successfully drained via this technique. It achieves results similar to open surgery with regards to the clearance of the infected tissue and radical debridement.
CONCLUSION
Spondylodiscitis resistant to antibiotics therapy may lead to progressive osseous destruction that necessitates surgical intervention. We should be aware of the diagnosis of spondylodiscitis when a patient has low back pain with a previous cardiac or dental procedure history. Endoscopic discectomy with debridement is a minimally invasive, safe, direct visualization and effective approach for treatment of infectious spondylodiscitis and is beneficial for symptom relief, rapid recovery and shorter duration of hospitalization.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
- magnetic resonance imaging
- mitral valve repair
- surgical procedures, minimally invasive
- debridement
- endoscopy
- chordae tendineae cordis
- dental procedures
- discitis
- diskectomy
- length of stay
- low back pain
- lumbar vertebra
- rupture
- surgical procedures, operative
- diagnosis
- heart
- spine
- pathogenic organism
- antimicrobials
- blood culture
- mitral valve leaflets
- robot assisted mitral valve repair
- granulicatella
- direct visualization



