-
PDF
- Split View
-
Views
-
Cite
Cite
Bassam Darwish, Mhd Belal Alsabek, Ameer Kakaje, A complicated pulmonary hydatid cyst resembling a tumour in an adult on PET scan: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa448, https://doi.org/10.1093/jscr/rjaa448
Close - Share Icon Share
Abstract
Complicated pulmonary cysts have a wide range of possible diagnoses with different approaches as they can be benign or malignant. They can resemble malignancies in symptoms and imaging, mainly on positron emission tomography (PET) scan, which can increase the false positivity. We present an infected hydatid cyst resembling a malignancy as it presented with weight loss in a smoker and had necrosis and malignance features on computed tomography and PET scans. However, serology tests and fine needle aspiration were suggestive of a hydatid cyst, which made this case quite unique. Other diagnoses should always be suspected even if the malignancy was highly likely due to other lesions can resemble malignancies.
INTRODUCTION
Pulmonary hydatid cysts can be asymptomatic or present with complications such as inflammation and infection. We present a patient who had a heterogeneous mass that resembled a malignancy in the lung. However, the patient had an unexpected hydatid cyst in the lung although the patient had the symptoms and characteristics of malignancy on computed tomography (CT) scan, and positron emission tomography (PET), as the lesion was complicated with infection.
CASE REPORT
A 50-year-old Syrian woman came with intermittent coughing for 4 months. The sputum was clear and recently became purulent with right chest pain and intermittent fever. She smoked 27 pack-years, and reported a weight loss of 5 kg and loss of appetite for the last 4 months. Family history was remarkable. Her physical examination revealed decreased breath sounds in the right mid lung field. Complete blood count (CBC) came with a high white blood cell (WBC) count of 12 600 × 109 cells/L with 73% being neutrophils. No tumour markers were checked.
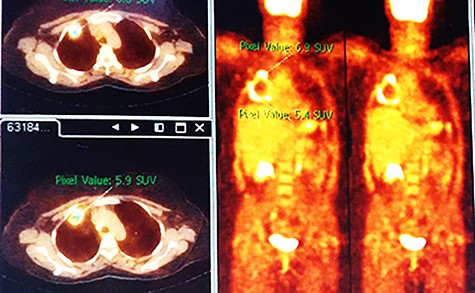
Chest X-ray (CXR) showed a heterogeneous density with irregular margins in the right lung (Fig. 1). CT scan demonstrated a heterogeneous mass that measured 5.5 × 6 × 7.8 cm with irregular thick margins. The mass was anteriorly located in the upper lobe of the right lung with air bubbles and necrosis (Fig. 2). Two lymphadenopathies were observed that measured around 2 cm each; one of which was in the hilum of the right lung and the other was located inferior to the right main bronchus. No other lesion was detected elsewhere. PET scan was also suggestive of malignancy as it demonstrated a heterogeneous mass with irregular margins which had irregular enhancement in the peripheral, suggesting hyper metabolic retention. The standardized uptake values (SUV) of the mass ranged between 4 and 7 with central necrosis and multiple gas bubbles. Multiple lymphadenopathies were also observed with different sizes ranged from 10 to 20 mm with SUVmax reaching 7 (Fig. 3). Bronchoscopy found an erythematous and oedematous opening of the anterior segment of the right upper lobe of the lung and epithelial dysplasia was found with bronchial lavage (BAL), but endobrachial biopsy was not conclusive.
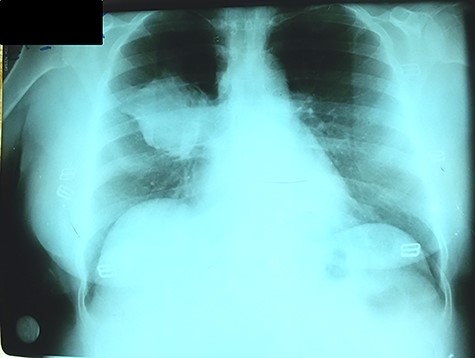
CXR with heterogeneous density with irregular borders in the right lung.
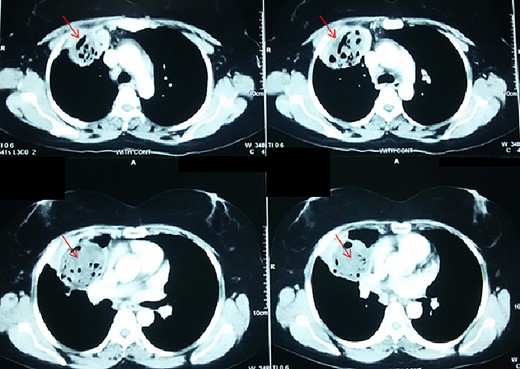
Thoracic CT-scan with the heterogenous mass having necrosis and gas bubbles (arrows).
As malignancy was suspected, a fine needle aspiration (FNA) through the chest wall was performed which found fragments of hyaline membranes and the germinal layer was lined with foam cells without viable scolex. Echinococcus granulosus antibodies test was performed and was found to be positive for 1/256 (negative up to 1/16). There was no other detectable lesion in the liver or any other organ. Surgery was indicated. At thoracotomy, a cystic mass was found with thick walls in the anterior segment of the upper lobe of the right lung. The mass was isolated by gauze towels soaked in hypertonic saline to safeguard against spillage of cyst contents into the pleural cavity (Supplemental video 1). The germ membrane was extracted as it was complicated with infection and pus. Three bronchocystic fistulas were then observed which were closed and the remaining cavity was stitched by capitonnage. A drainage tube was then installed in the pleural cavity. Postoperatively, 10 mg/kg of albendazole was prescribed. The CXRs were unremarkable for the next 6 months.
DISCUSSION
Hydatid cysts can affect all organs, with the liver and lungs being the most common [1, 2]. Hydatid cysts have many presentations although the majority are asymptomatic and hence found incidentally [1, 3]. However, they can rupture, which can cause symptoms of productive cough, coughing out cystic contents, haemoptysis and chest pain. The diagnosis is usually easy by typical radiological findings, especially if they are accompanied with hepatic hydatid cysts [3]. However, when they are complicated with infection, the diagnosis can be quite challenging as the clinical and radiological findings become atypical and resemble lung malignancies [1, 2, 4]. That is why diagnosis should not be excluded despite having features of malignancy.
In case of high suspicion, bronchoscopy becomes a powerful tool as visualization of whitish endobronchial lesions can be observed, which is hard to be misdiagnosed with necrotic bronchial carcinoma. In addition, biopsies can be performed with bronchoscopy which can make the definitive diagnosis [5].
When using PET-scan, lesions that demonstrate Fludeoxyglucose (FDG) retention and have SUVmax higher than 2.5–3 are approached as malignancies [6]. However, results that are false positives are expected as many conditions can cause FDG retention and enhancement such as granulomatosis, inflammation and infection, with tuberculosis, sarcoidosis and parasite diseases being among the most common causes [7]. One study had 15 cases of hydatid cysts which mimicked malignancies on PET-scan and was speculated that local inflammation by the ruptured cyst was the reason for the resemblance [4]. In our case, the cyst ruptured and had infection, which can explain the resemblance of malignancy on PET scan. In another study, the quite opposite to our case was observed; a lung carcinoma mimicked hydatid cyst with positive serology for echinococcus granulosus, which can further confirm the resemblance that can occur [8]. FNA should be avoided in hydatid cysts to avoid rupture and anaphylaxis in the patient, which is why they should be excluded before any procedure even in cases of apparent malignancy. FNA was conducted in our case as malignancy was suspected, not echinococcus granulosus. PET scan is an expensive imaging and therefore test for echinococcus granulosus should have been conducted before, particularly that in Syria financial burden can limit in some extent medical treatment in some cases [9].
In conclusion, complicated lung cysts diagnosis imposes major challenges, but other possible diagnoses should also be considered such as having a hydatid cyst as they can resemble malignancies when complicated mainly in epidemic countries. Although PET scans can be suggestive of malignancy in the lungs, benign lesions and parasitic cysts should not be excluded as PET scan can increase false positivity, mainly when the lesion is inflamed. This case is particularly important when cases are highly suspected to be a malignancy from presentation and imaging as they can sometimes be misleading.
ACKNOWLEDGEMENT
This work was conducted in Al Mouwasat University Hospital.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Informed consent was taken for this research. Our study ethical aspects were reviewed and approved by Damascus University deanship, Damascus, Syria.
CONSENT FOR PUBLICATION
Consent for using and publishing the data was taken before participating in the research.
AVAILABILITY OF DATA AND MATERIALS
The data can be made available upon reasonable request.
CONFLICT OF INTEREST STATEMENT
We have no conflict of interest to declare.
FUNDING
No funding was received for this study.
References
Author notes
Bassam Darwish is the guarantor for the images and the case.



