-
PDF
- Split View
-
Views
-
Cite
Cite
Zain Douba, Judy A Sinno, Haya Jawish, Nour Hakim, Abdullah Mouselli, Mohamad B Shihade, Mohamed A Abdullah, Samer Alhames, Unusual localizations of hydatid cysts: a rare case report from Syria, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa438, https://doi.org/10.1093/jscr/rjaa438
Close - Share Icon Share
Abstract
Hydatid disease (HD) is an infection with the metacestode stage of the tapeworm Echinococcus. It is commonly seen in South America, The Middle East, Eastern Mediterranean, Africa and China. Hydatid cysts usually affect the liver followed by the lungs. Involvement in other organs has been reported. However, in the majority of the cases, cysts are localized in one organ or one region. We report a rare case of a 36-year-old woman who presented to the hospital in Syria with long-standing history of non-specific abdominal pain. Computerized tomography showed several hydatid cysts in the liver, spleen, left lung, mediastinum (adjacent to the aortic arch), both breasts and above the right gluteal muscles.
INTRODUCTION
Cystic hydatidosis or echinococcal disease is an infection caused by Taenia Echinococcus [1]. The primary hosts for this disease are dogs and cattle. Human transmission occurs by ingesting food or drinking water infected with the parasite’s eggs or through direct contact with the hosts. HD can affect any organ; the liver is affected in ~70% of cases, followed by the lungs [2]. Extrapulmonary and extrahepatic localizations are rare and have been reported in 2% of hydatidosis patients [1].
Hydatid cysts are usually asymptomatic, and the symptoms usually develop depending on the location and the size of the cysts [3]. In case of liver involvement, a patient presents with abdominal pain, nausea and vomiting. When the cysts are located in the lung, an HD patient presents often with cough, fatigue and, in some cases, shortness of breath. Hydatid cyst can lead to life-threatening complications such as cyst rupture with potential anaphylactic shock, new cysts spread and bacterial infection.
In this article, we will present a case of a young woman who presented with multi-organ involvement with hydatid cysts.
CASE REPORT
A 36-year-old woman presented to the emergency room in Syria with 1-year history of right upper quadrant pain. The pain increased in the weeks prior to admission. The patient denied fever, chills, nausea or vomiting. Past medical history was positive for treated pulmonary tuberculosis 2 years ago.
On physical examination, the patient was malnourished and looked chronically ill. Abdominal examination showed several palpable, clear edge masses in the liver with no tenderness. Lung auscultation reported decreased breath sounds in the base of the left lung. A swelling was detected in the right buttock with no erythema or tenderness. Breast exams showed bilateral mobile cystic lesions in both breasts. The nipples were normal, and there was no axillary or cervical lymphadenopathy.
Laboratory exams revealed microcytic hypochromic anemia, slightly elevated leukocytes (10.2 × 109/l, Ref. 3.6–10 × 109/l) and no eosinophilia. Liver enzymes were within normal limits other than elevated alkaline phosphatase (130 IU/l, Ref. 34–104 IU/l). Indirect hemagglutination test for HD (Weinberg) was strongly positive (1/1280, Ref. 1/160).
Abdominal ultrasound delineated multiple cystic lesions in the liver and the spleen. Computed tomography (CT) scan showed up to six rounded homogenous low-density cysts in both lobes of the liver, ranged from 0.15 to 0.17 m, and one large cyst in the spleen, containing multiple peripheral small vesicular cysts (Fig. 1). CT scan showed a 0.03 × 0.07 m cyst in the upper mediastinum, adjacent to the aortic arch (Fig. 2A); two rounded well-defined homogenous cysts in the lower lobe of the left lung, measured 0.17 × 0.17 m, and in both breasts (Fig. 2B and C) and a single large 0.2 × 0.13 m oval homogenous cyst above the right gluteal muscles (Fig. 3).

Abdominal CT scan reveals: six rounded homogenous low-density cysts in the liver, measuring from 0.15 to 0.17 m. A large rounded cyst in the spleen, containing multiple peripheral small vesicular cysts.
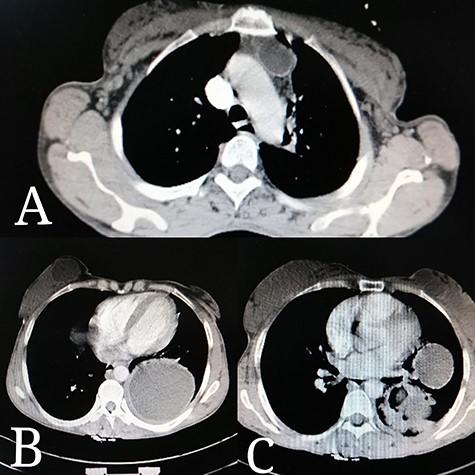
Thoracic CT scan reveals: (A) a 0.03 × 0.07 m cyst in the upper mediastinum, adjacent to the aortic arch. (B) A rounded cyst in the right breast. (C) Few rounded cysts in the left breast. (B, C) Two rounded homogenous cysts in the lower lobe of the left lung, measuring 0.17 × 0.17 m.
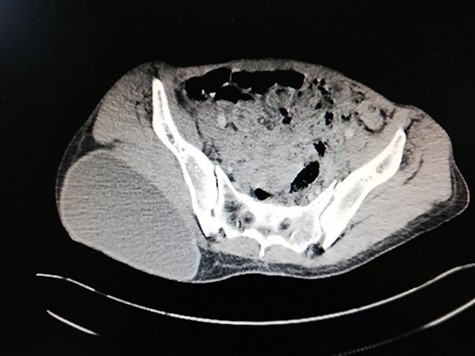
Pelvic CT scan reveals: a large oval homogenous cyst, above the right gluteal muscles, measuring 0.2 × 0.13 m.
The patient was admitted to the hospital for symptoms management. She was started on weight-based Albendazole (0.4 g twice a day). The patient improved clinically and was taken to the operating room for left anterolateral thoracotomy. The surgical field was covered to prevent the spillage of parasites into the surrounding tissue. The cyst was punctured and aspirated. The aspirated fluid was clear and colorless. Then, the scolicidal agent (hypertonic saline 30%) was instilled into the cyst cavity and left for ~15 minutes. The scolicidal agent was then aspirated and the cyst contents were evacuated. The cavity was explored carefully for any gross communication with the bronchus; a small bronchial fistula was found and closed. The mediastinal pleura was then entered and the mediastinal cyst was enucleated. One thoracic drain was placed.
The bilateral breast cysts were excised by enucleation. The right gluteal cyst was excised by enucleation as well and a drain was placed. The operation lasted for 5 hours with no need for blood transfusion.
Following surgery, the patient was restarted on Albendazole and a second operation on the abdomen was recommended 6 weeks later. However, the patient was lost for follow-up during the COVID pandemic.
DISCUSSION
Hydatid disease is a parasitic infection caused by the Echinococcus granulosus and seen endemically among animal-raising communities. Hydatid cysts can involve different organs, mostly lung and liver, but it is also reported in other areas. They are usually asymptomatic depending on the size and the location involved. Musculoskeletal hydatid cysts, including gluteal cysts, and breast cysts are very rare and usually present with painful masses in the breast and the gluteal region. It usually presents concomitantly with hydatid cyst in other organs [4]. In our case, the patient had several cysts causing both localized and systemic symptoms.
Hydatid cyst is usually diagnosed by history, physical examination, imaging and serological tests. Patients usually live in a cattle-raising rural area with close animal contact. Ultrasound and CT can help diagnose the hydatid cyst in the liver and the lung [5]. Different modalities might be more helpful in other locations such as the breast and the gluteal muscles. Total surgical excision is indicated for symptomatic cysts, especially if the size is more than 0.05 m. Antihelminthic drugs, such as Mebendazole and Albendazole, are usually given pre- and postoperatively to reduce risk for local recurrence [6].
Hydatid cysts can cause several complications if they were poorly managed. Complications may range starting from cystic rupture leading to anaphylactic shock. Furthermore, the spread of multiple ‘daughter’ cysts can cause secondary infection and fistula formation [2].
During the recent years, and because of years of war, patients in Syria have been presenting with advanced stages of their diseases as medical care and communication between cities have been disrupted. We have been witnessing several advanced and symptomatic cases of hydatid cysts in multiple and rare locations similar to this case where the patient had 12 cysts in the both breasts, mediastinum, right gluteal, spleen, left lung and the liver.
Our patient was discharged on Albendazole and then unfortunately lost for follow-up given the COVID crisis.
ACKNOWLEDGEMENTS
We want to thank Miss Noor Ajam for her support. We are grateful to the CME Office in Faculty of Medicine, University of Aleppo.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



