-
PDF
- Split View
-
Views
-
Cite
Cite
Metasebia W Abebe, Tezazu Tefera, Mengistu G Mengesha, Mulualem W Mengesha, Sisay Teshome, Case series of hyena bite injuries and their surgical management in a resource-limited setup: 1-year experience, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa446, https://doi.org/10.1093/jscr/rjaa446
Close - Share Icon Share
Abstract
Animal bites are a significant cause of morbidity and mortality and pose a major public health problem worldwide. Children are reportedly the most common victims of animal bites. Bites may be limited to superficial tissues or lead to extensive disfiguring injuries, fractures, infections and rarely result in death. Recently, human injuries caused by non-domesticated animals are increasingly common as ecosystems change and humans encroach on previously wild land. Wild animals like hyenas have been reported to prey on humans and cattle in parts of Africa. Discussed here are four children out of 11 patients that presented with hyena bites—the children had severe bites to the face and head with extensive soft tissue loss, fractures and concomitant severe infections that led to high mortality, indicating the necessity for advanced intensive care and multidisciplinary treatment needed in such situations.
INTRODUCTION
Animal bites are a significant cause of morbidity and mortality and a major public health problem worldwide. Outcomes of patients depend on a variety of factors including the type of animal causing the bite, status of the animal (rabid or healthy), host factors (age of the patient, nutritional status and overall health condition) and access to appropriate health care facilities as well as expertise [1–4]. A major problem frequently associated with animal bite injuries is the transmission of human rabies an endemic problem in Africa and Asia [1, 2, 5].
The extent of injury in animal bites may be limited to superficial tissues or involve deeper structures that can lead to permanent disfigurement requiring reconstructive surgery, bony fractures resulting in disability, severe infections as rabies or from the oral flora of the biting animal, and in rare cases attacks may be fatal [1–3, 6]. Though the commonest animal bites worldwide are from dogs, numerous other animal species that are domesticated or non-domesticated have the potential to bite humans [1, 2, 5–7]. The most common victims of dog bites are children, up to 50% of them present with bites to the face which may be mainly due to the provocative behavior of children toward animals and their short stature that makes their faces accessible to animal’s reach. In addition to the injuries to these soft and hard tissues following animal bites, the introduction of a variety of infectious organisms to the bite wound is a serious concern [3–7].
There are many people in low- and middle-income countries that die before receiving adequate medical care and many others that are undocumented after animal bite injuries. On top of severe physical trauma and potentially permanent disfiguring wounds, bite victims also often suffer from emotional and psychological trauma [4, 7].
Animal attacks on people are also a huge medico-social problem resulting in millions of injuries and thousands of deaths all over the world. The tremendous medical and financial costs from both fatal and non-fatal animal attacks have a significant impact on public health [4]. These wild animal attacks and the complex injuries that result may pose a challenge to surgeons practicing in resource-limited settings [8]. Therefore, we believe this series of cases can show the magnitude of the problem and show the management approach implemented in the resource-limited setting with all the logistical, as well as human resource limitations. We also believe it can serve as a tool for a better approach and better preparation for such cases that present in the future. To our knowledge, in Ethiopia, if not in the world, this is the first case series study done on hyena bite.
CASE SERIES
A total of 11 hyena bite cases presented to our institution in 2019, eight (72.7%) of the patients were in the pediatric age group, which is under the age of 18 years. Six (54.5%) of the patients were male. The majority (81.8%) were from the rural area presented with severe bites to the head and neck region mainly over the face with only two (18.2%) patients presenting with lower extremity bites. All of the patients had extensive soft tissue injuries with five (45.5%) of them having concomitant bony fractures. Prolonged hospitalization with a mean duration of stay of 17 days and complex surgeries were required for all the patients whereby three patients died which makes mortality rate of 27% during the course of treatment. Four (36.4%) of patients reported that they had more than two previous hyena attacks before their current attack. Three (27.2%) patients reported that they were attacked during the broad daylight. All patients received tetanus antitoxin, anti-rabies vaccine and broad-spectrum antibiotics for at least one week.
We have presented here four of the 11 cases that were in the pediatric age group and had bites over the face and head.
Case 1
A 2-year-old female child from a rural area in the southern region of Ethiopia presented 18 h after sustaining a hyena bite while playing outside in her neighborhood. The bite was over the head and face with a compound depressed skull fracture with visible dural tear and oozing of brain tissue as well as a pre-auricular laceration. Proper irrigation and debridement with removal of fragments of bone and dura-plasty were done for 3 × 2 cm dura defect. The patient was put on antibiotics and discharged improved (Fig. 1).

A 2-year-old female patient with hyena bite to the head resulting in a compound depressed skull fracture.
Case 2
A 4-year-old male child from a rural area in the southern region of Ethiopia presented three and a half hours after sustaining a hyena bite to his face while playing outside in his neighborhood. He had soft tissue loss over the nose, eyelids, cheek and lip over the right hemiface, there were zygomatic bone fracture and loss of nasal bones. In the absence of microsurgical services and state of malnutrition of the child, he was admitted and given antibiotics and nutritional support for a couple of weeks and bilateral pedicled deltopectoral flap and forehead flap was used to cover the soft tissue defects over the face. The patient was then put on antibiotics but died of uncontrollable sepsis and multiple organ failure following a hospital-acquired pneumonia after 3 weeks of hospital stay (Fig. 2).

A 4-year-old male patient with hyena bite to the face resulting in loss of nose, eyelids, cheek and lips.
Case 3
A 7-year-old male child from a rural town in the Oromia region of Ethiopia presented 3 h after sustaining a hyena bite with soft tissue injuries over his face with the loss of nasal bone and exposed bone over the upper third of the nose. Irrigation and debridement with coverage of exposed bone with paramedian forehead flap were done. The patient then received antibiotics and was discharged improved (Fig. 3).

A 9-year-old male patient with hyena bite to the face resulting in exposed nasal bone.
Case 4
An 8-year-old female child from a rural area in the southern region of Ethiopia presented 5 h after sustaining a hyena bite to her face with extensive soft tissue injury and nasal bone loss with bilateral post-traumatic vision loss while she was fetching water at a nearby riverside. Even though debridement and irrigation were done twice and she was put on antibiotics, the patient died of severe septicemia from the extensive wound in the hospital after she stays for a couple of weeks (Fig. 4).
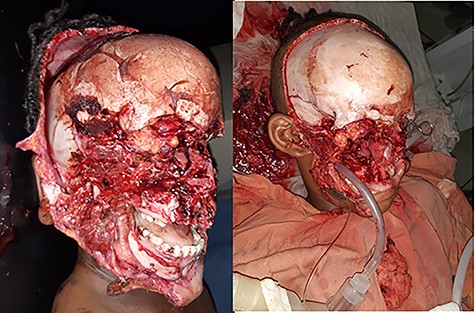
An 8-year-old female patient with hyena bite to face, eyes, nose and scalp.
DISCUSSION
Millions of victims of animal bites receive treatment annually posing a major public health problem with significant morbidity and mortality [4], which is reflected with a high mortality rate of 27.3% in our case series. Even though data from low- and middle-income countries is frequently fragmented and incomplete, human injury resulting from encounters with non-domesticated animals is increasingly common throughout the world [1, 2, 5] particularly with the changing climate and ecosystems and the increasing human population encroaching on previously wild land which is corroborated by the hyena bites of our patients that occurred both in the day and night time not so far from their living house and the fact that 36.4% of our cases had a history of more than two hyena bite attacks before the current bite will strengthen the scenario.
Wild animals such as hyenas either rabid or healthy have been known to attack and kill humans and prey on domestic livestock in Africa [9, 10]. In line with this, our hyena bite case series depicts the situation in one of the regional referral hospitals in the southern part of Ethiopia, HUCSH, which provides a variety of multidisciplinary sub-specialty-based surgical services including plastic and reconstructive, orthopedic and neurosurgery despite the limited resources.
Common sites of injury are stated as extremities since humans tend to try and fend off the attacks using their hands and feet [3, 5–7], which was also seen in the adult cases in our series. Children tend to present with bites to the head and neck region because of their short stature and provocative behavior [3, 5–7]. About 81.8% of our case series were children who were unable to fend off a hyena in addition to their size inevitably making the site of the bite on their head and neck region.
An animal bite wound can be characterized by various types of injuries like abrasions, puncture wounds, avulsions, lacerations and crush injuries along with underlying fractures, foreign bodies and tendon and nerve injuries [7]. This was also seen in our series with multiple cases of a skull, mandibular and zygomatic fractures and extensive soft tissue injuries with tissue loss requiring complex reconstructions.
The tremendous medical and financial costs from both fatal and non-fatal animal attacks have a significant impact on public health [4], more so for patients in low-income countries like Ethiopia, where there is no health financing system and patients have to pay out of pocket for medication and services by selling their cattle. This will compromise their livelihood especially when they present with complex injuries that require an extended length of hospital stay and advanced care. The mean number of days of admission in our case series was 17 days which is a very long stay for the majority of Ethiopian population and can cause economic distress for the patients.
These wild animal attacks and the complex injuries that result may pose a challenge to surgeons practicing in resource-limited settings [8]. In the absence of microsurgical reconstructive services, appropriate imaging studies and limited resources, many of the cases in our series were a challenge to manage for the surgeons indicating the need for better resource allocation, better critical care practices, identification of microorganisms and procurement of necessary equipment along with staff training.
ACKNOWLEDGEMENTS
We would like to extend our gratitude to the patients and patients’ families who allowed us to use their photo for publication. We are also thankful to HUCSH and all staff members who were involved in lending support during the course of data collection.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.



