-
PDF
- Split View
-
Views
-
Cite
Cite
Obed Rockson, Christine Kora, Abdelbassir Ramdani, Badr Serji, Tijani El Harroudi, A case report of an unusual caecal metastatic location of a primary cervical squamous cell carcinoma , Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa443, https://doi.org/10.1093/jscr/rjaa443
Close - Share Icon Share
Abstract
Squamous cell carcinoma (SCC) of the colon is a rare malignant tumor occurring as either a primary or secondary lesion. Few cases of metastatic or secondary colonic SCC have been published. We report an unusual case of a 59-year-old female patient who was treated by Wertheim hysterectomy and adjuvant chemoradiation for stage IIB SCC of the uterine cervix. Two years later, she developed a metastatic location in the caecum causing an acute intestinal obstruction. She underwent an emergency open right hemicolectomy with ileocolic anastomosis and resection of two nodules of the umbilicus and the right parietal peritoneum. Histopathological examination confirmed a triple metastatic location of SCC. She is disease-free 11 months after surgery. We discuss the clinicopathological features, management strategies, and the prognosis of this rare entity.
INTRODUCTION
Metastatic squamous cell carcinoma (SCC) of the digestive tube is relatively uncommon. In patients with advanced SCC of the uterine cervix treated by radiation, 9–27% may develop distant metastasis [1]. Usually, the disease progress through metastasis within the first two years of treatment and is associated with an overall poor prognosis [2]. Surgical resection is the main therapeutic modality, while the role of chemotherapy and radiotherapy remain ambiguous [3]. We report a case of SCC of the cervix metastasizing to the caecum and resulting in acute bowel obstruction. Physicians should be aware of the unusual metastatic locations of cervical SCC to the caecum and must be considered in the differential diagnosis of acute abdomen in patients with cervical cancer.
CASE REPORT
A 59-year-old female patient with a history of hypertension was diagnosed with a well-differentiated stage IIB SCC of the cervix according to the International Federation of Gynaecology and Obstetrics classification where she underwent a total abdominal hysterectomy and bilateral salpingo-oophorectomy followed by adjuvant chemoradiation. She received a weekly dose of cisplatinum along with external and internal beam radiotherapy. There was no evidence of locoregional recurrence during her follow-ups and serial Papanicolaou smears were negative.
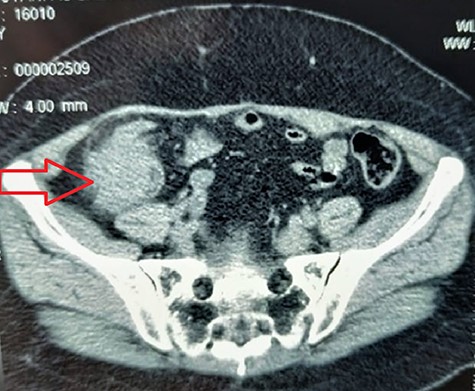
Two years later, she was admitted to the emergency department (ED) for acute bowel obstruction, with generalized abdominal pains, worsen in the right iliac fossa (RIF) associated with vomiting of gastric content, and without passage of stools or flatus. On physical examination, her vital signs were stable. Abdominal examination revealed a slight tenderness in the RIF, exaggerated bowel sounds with a 4 cm × 4 cm hard mobile lump in the RIF. Digital rectal examination revealed an empty rectal bowel. All the lymph node areas were disease-free. In the ED, abdominal computerized tomography (CT) scan revealed an intraluminal-caecal mass, measuring 43 mm in diameter, rounded in shape, tissue density, homogeneous, discreetly enhanced by the contrast product with no distant metastatic spread (Fig. 1).
Given the evidence of acute bowel obstruction, an exploratory laparotomy was performed which revealed a single hard, mobile mass of the caecum of size 5 cm × 5 cm. An extended right hemicolectomy with resection of two nodules in the umbilical and right parietal peritoneum and manual end-to-end ileo-transverse anastomosis was performed (Fig. 2). The postoperative course was uneventful and the patient was discharged on day 3. Histopathological examination of the resected specimen concluded a triple secondary localization of SCC in the caecum and both the nodules of the umbilicus and parietal peritoneum (Fig. 3A, B, and C).
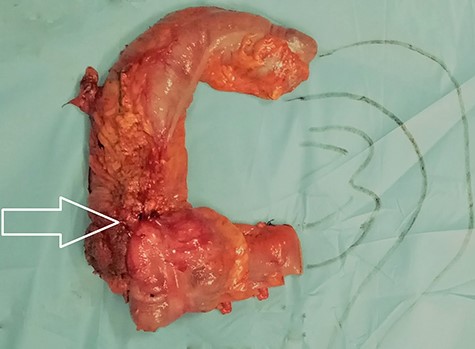
Surgical specimen of the resected right colon with the tumor (white arrow).
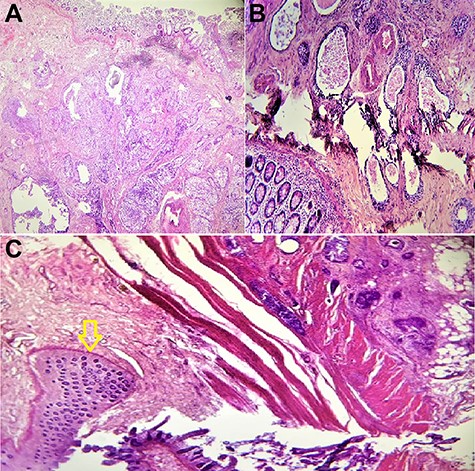
Microscopic findings: (A and B) the colon mass was composed of well-differentiated squamous carcinoma cells; (C) tumor cells are voluminous rounded anisocytosis marked with basophile cytoplasm with blurred contours (yellow arrow); hematoxylin and eosin staining; magnification ×100.
Following discussion in a multidisciplinary team meeting, the patient was addressed for complementary adjuvant chemotherapy where she received a combined carboplatin 540 mg and Gemcitabine 700 mg without radiotherapy. An 11 months follow-up period has shown no signs of recurrence.
DISCUSSION
Due to the glandular structure of the colorectal lining, about 90% of colon cancers are adenocarcinomas. The remaining 10% of tumors consist of SCC, neuroendocrine tumors, undifferentiated carcinomas and lymphomas [4]. The primary tumors known to metastasize to the colon include the breast, lung, kidney, ovary, and malignant melanomas [5]. The literature regarding these tumors is limited, with most articles being solitary case reports. In the past three decades, a total of nine cases of metastatic carcinoma cervix to the colon have been reported [2–6].
It occurs on average around the fifth decade with male predominance (sex ratio: 2). It is mostly located in the caecum and right colon, unlike adenocarcinomas [7]. The symptoms are indistinguishable from that of the adenocarcinoma’s counterpart. Haematochezia and abdominal pains, as well as non-specific symptoms such as abdominal distension, and vomiting, are common clinical features. Sometimes, the diagnosis is made at the stage of complications, with symptoms suggestive of bowel obstruction or perforation leading to peritonitis [2, 7].
As a primary tumor, its pathogenesis is still unclear, it appears to develop from a multipotent stem cell or Malpighian metaplasia secondary to chronic mechanical irritation. Williams et al. [8] established three diagnostic criteria for primary SCC to help distinguish it from metastatic SCC: the non-existence of a non-colonic primary SCC, eliminating the presence of an underlying squamous-epithelial lined fistula to the tumor site and exclusion of SCC of the anus spreading into the rectum
None of these three criteria were present in our patient to diagnose possible primary colonic SCC. Moreover, with the history of SCC of the cervix, the most likely diagnosis was a metastasis of cervical cancer that was confirmed after histopathologic analysis. As a secondary tumor, it arises through metastasis, either by one of these four methods: transperitoneal, hematogenous, lymphatic or transluminal [5].
The optimal treatment for this condition remains controversial, with no available data comparing the efficacy of the different treatment options available. Currently, the treatment is based on that applied for adenocarcinomas cases, which is predominantly surgery followed by chemotherapy and/or radiotherapy. Surgical resection and debulking of the tumor is the gold standard. The outcomes of adjuvant treatment are random. Chemotherapy could also be employed as a palliative treatment. Many authors agree to various treatment regimens including 5 fluorouracil (5FU)/mitomycin C, 5FU, 5FU/cisplatin, capecitabine/cisplatin, capecitabine and raltitrexed/oxaliplatin [3, 4]. Zhao et al. [3] believe gemcitabine may be a treatment option in the neoadjuvant and/or adjuvant chemotherapy setting. The efficacy of radiotherapy, with or without chemotherapy, has not been established due to the rarity of the tumor.
The prognosis of the disease is poor with the overall survival is less than a year [1, 2, 5]. Early detection with prompt intervention is the key factor required in the successful management of these tumors and to improve the overall survival of the patient. Follow-up is aimed at detecting recurrence, as these tumors are more aggressive than other histological types.
AUTHOR CONTRIBUTIONS
All the authors testified to the care of the patient and the writing of the manuscript. The authors have read and approved the final version of the manuscript.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
REFERENCES
- cancer
- squamous cell carcinoma
- immunologic adjuvants
- pharmaceutical adjuvants
- hysterectomy
- surgical procedures, operative
- umbilicus
- cecum
- cervix uteri
- colon
- surgery specialty
- peritoneum, parietal
- intestinal obstruction, acute
- squamous cell carcinoma of cervix
- radiochemotherapy
- colectomy, right
- ileocolic anastomosis
- histopathology tests



