-
PDF
- Split View
-
Views
-
Cite
Cite
Yi Ying Law, Rhea Patel, Marianne Cusick, Jeffrey L Van Eps, A case of colonic intussusception and obstruction secondary to giant colonic lipoma, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa429, https://doi.org/10.1093/jscr/rjaa429
Close - Share Icon Share
Abstract
Lipomas are benign soft tissue tumors found throughout the body including the gastrointestinal (GI) tract. Colonic lipomas are typically asymptomatic, incidentally identified during endoscopy or at the time of autopsy. However, giant lipomas larger than 4 cm usually manifest symptoms such as abdominal pain, obstruction, melena or intussusception. The transverse colon is the least common location for colonic lipoma. We report on a 54-year-old man with acute large bowel obstruction secondary to a long segment colo-colonic intussusception from a giant lipoma originating in the transverse colon. The diagnosis was suggested by advanced imaging and confirmed on endoscopy. He was treated successfully by laparoscopic extended right hemicolectomy with ileocolonic anastomosis. This case highlights the complexity of presentation and surgical management of large bowel obstruction and colonic intussusception, as well as the rare entity of giant colonic lipoma.
INTRODUCTION
The gastrointestinal (GI) tract is fertile ground for an assortment of soft tissue lesions both benign and malignant including adenomatous/hyperplastic polyps, endometriomas, rare melanoma or sarcoma and many more. Lipomas are nonepithelial, benign fatty tumors commonly found subcutaneously on the trunk or extremities and throughout the GI tract. Though typically asymptomatic and incidental, they may present with abdominal pain, obstruction, melena or occasionally, intussusception [1, 2]. Symptoms often correlate with size, and 75% of patients with a lipoma larger than 4 cm will experience some form of symptoms [3]. The most common locations for colonic lipomas are the ascending colon/cecum (45%), followed by sigmoid colon (30.3%), descending colon (15.2%) and finally transverse colon (9.1%) [5]. Unlike children, intussusception in adults is most frequently caused by a malignant lead point. Giant lipomas (>4 cm) are the most common benign tumors to cause adult intussusception [3, 4]. Intussusception may be asymptomatic or it may present with intermittent or complete bowel obstruction, which requires urgent surgical treatment. Advanced imaging such as computed tomography (CT) or magnetic resonance imaging (MRI) characterize intussusception well and can be diagnostic, with the ability to identify masses acting as a lead point.
CASE REPORT
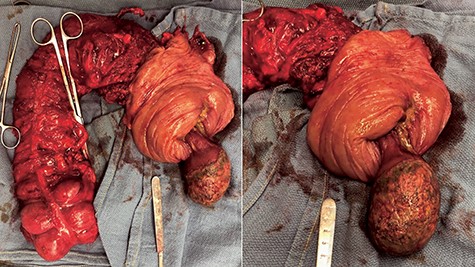
A 54-year-old man presented to his gastroenterologist with a 4-week history of worsening crampy abdominal pain associated with abdominal distention and obstipation. He was admitted urgently to the hospital after CT imaging revealed an evolving large bowel obstruction from transverse colonic intussusception likely secondary to a colonic mass lead point (Fig. 1). The patient underwent colonoscopy, but dusky nonviable mucosa was seen at the leading edge of the intussusceptum (Fig. 2), so no attempt was made to traverse it and the patient was taken for emergent surgical treatment. Using a hand-assisted laparoscopic approach, the cause of obstruction was confirmed to be a long segment of intussuscepted proximal transverse colon traversing the entire splenic flexure into descending colon, with a boggy mass acting as the lead point. The transverse colonic intussusceptum was carefully milked backward from within the descending colonic intussuscipiens to its natural anatomic position. Despite return of pink, viable colon appearance after a decompressive colotomy, some serosal abnormalities and congestion of the right colon from severe distention warranted its resection. An extended right hemicolectomy was performed with a distal transection margin 10 cm distal to the colonic mass origin, followed by stapled side-to-side, functional end-to-end ileocolonic anastomosis. The resected specimen was opened intraoperatively, revealing a large, pedunculated, polypoid mass with soft center consistent with colonic lipoma (Fig. 3). The patient recovered well, with return of bowel function on postoperative Day 3 prior to discharge home. Histopathology confirmed a 9.5 × 5.5 × 4.5 cm submucosal lipoma (Fig. 4) and 12 benign lymph nodes.
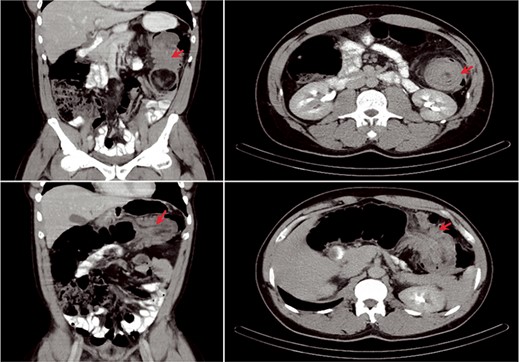
CT appearance of colonic intussusception (arrows) in the left upper quadrant secondary to colonic mass.
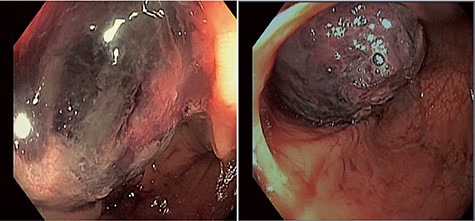
Colonoscopic images of the colonic intussusceptum with an ischemic, dusky mass lead point secondary to mucosal edema and venous congestion.
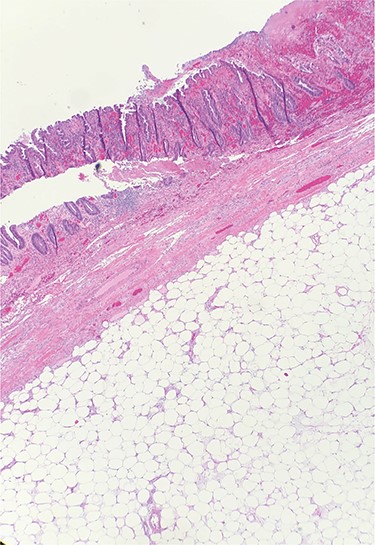
Hematoxylin and eosin (H&E) staining of colonic specimen revealing a submucosal lipoma.
DISCUSSION
Lipomas of the GI tract are not uncommon, but they rarely cause symptoms such as bowel obstruction requiring emergent resection, especially at the transverse colon. Those who present with symptoms rarely experience intussusception, which is usually limited to one segment and typically affects the right colon [1, 7]. The early diagnosis of intussusception in adults is challenging, lacking the classic triad of abdominal pain, palpable abdominal mass and hematochezia as often seen in children. CT imaging can facilitate diagnosis with a sensitivity of 58–100%, with typical radiographic appearance known as a ‘target sign’ or ‘doughnut sign’ [6]. If large enough, an ovoid mass will be seen on CT ranging from 40 to 120 Hounsfield units (HU), typical of fat [3]. MRI can also distinguish fatty lipoma from surrounding structures. Ultrasound can also be used, particularly in children, and a hyperechoic submucosal lesion on endoscopic ultrasound is diagnostic for lipoma [1].
It is important to distinguish benign lipomas from other subepithelial lesions found on endoscopy, such as leiomyoma or gastrointestinal stromal tumors (GIST). Findings on colonoscopy include the ‘pillow sign’ (soft lesion with mucosal indentation resembling a pillow when pressed with closed biopsy forceps, Fig. 5A), and the ‘naked fat sign’ (extrusion of fat after biopsy, Fig. 5B) [6, 7]. While the majority of colonic lipomas present as sessile or pedunculated submucosal lesions, 10% are subserosal and multiple lesions are reported in up to 20% of cases [8]. Biopsy may be required in the setting of ambiguous endoscopic findings. Positive naked fat sign is diagnostic for lipoma and does not require excision unless complicated by refractory bleeding, whereas equivocal findings require histopathologic review.
![Endoscopic signs of colonic lipoma including (A) pillow sign and (B) naked fat sign with protruding submucosal fat after biopsy, reconfigured from Zimmer [7].](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2020/10/10.1093_jscr_rjaa429/2/m_rjaa429f5.jpeg?Expires=1773968546&Signature=CLORTSpG-ofp60yhqJkbIDiL17ncoqbMmGt4psxVB1BaoY14KipMgLho4tPYSNbxU7a8QF9Ghn3HEIeDU3MbQWXMlL-xLjZbS4dnrd3MKxj664Z3bBs41qSXMP6tcA7peX~Q9DREzCXqA8VpybqqEJFxIoBD4-DIN0bVl4llwhcx0-wEWDXHunOnsAoMP5KGZSWFuTl1o5a0NB9OxIOaHYUnW7L2M02pr05OdFttvVTlvTnocjj2d7VH2byex9ONQZc2~k~12hTLzwedfz8PUwQFjz7qQrIPARJmn2C1KQ1n4I9TMWMTuqcAWGPGGGPV1ck2DdOVXrlliNecEA-Yhw__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
Endoscopic signs of colonic lipoma including (A) pillow sign and (B) naked fat sign with protruding submucosal fat after biopsy, reconfigured from Zimmer [7].
In the setting of adult intussusception, malignant tumors remain highest on the differential, limiting the role of some preoperative diagnostic tests such as endoscopy, which may otherwise be useful for obtaining tissue diagnosis in the absence of obstruction. However, since histopathological examination is required for diagnosis, surgical resection is typically required and is recommended for symptomatic lipomas or those that pose a diagnostic challenge. Lipomas can be resected endoscopically or surgically. Techniques for an endoscopic approach include lipoma ‘unroofing’ loop-assisted-snare dissection, or dissection techniques such as endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD). A recent systematic review demonstrated that all four approaches provided similar clinical remission rates, but loop-assisted-snare technique and deeper dissection are associated with more adverse events including bleeding and perforation [9]. More radical surgical resection is recommended when giant lipomas are complicated by intussusception or bowel obstruction [3]. Preoperative diagnosis of a benign etiology allows for ‘milking’ back the intussusception, facilitating a more limited resection [6]. The use of minimally invasive approaches is associated with improved pain control, shorter hospital stay and recovery period [10]. Such minimally invasive techniques should be employed whenever feasible and our case provides additional data regarding its safety and efficacy even in the setting of obstruction.
CONFLICT OF INTEREST STATEMENT
None declared.



