-
PDF
- Split View
-
Views
-
Cite
Cite
Atta Nawabi, Sumaiya Serwar, Jeffrey Klein, Perwaiz Nawabi, Nadia Nawabi, Diane Cibrik, Nonoperative management of gastrointestinal bleeding after a simultaneous pancreas and kidney transplant, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa433, https://doi.org/10.1093/jscr/rjaa433
Close - Share Icon Share
Abstract
With a shift toward enteric drainage techniques, the complications associated with simultaneous pancreas and kidney (SPK) transplant have also changed. Gastrointestinal (GI) bleeding is one of the most common complications associated with SPK. This case report describes the treatment of a postoperative GI hemorrhage using the push endoscopy technique. A 48-year-old male underwent an uneventful SPK transplant with entero-systemic drainage and developed hematochezia. The push enteroscopy technique was utilized to treat the bleeding ulcer. Historically, the use of the push enteroscopy technique to treat GI bleeding from the small bowel is not described in the literature. One of the limitations of duodenojejunostomy is that standard endoscopy cannot be readily used to visualize the duodenojejunostomy. However, the use of push enteroscopy may prove to be a minimal invasive and cost-effective intervention for GI bleeding after SPK.
INTRODUCTION
Within 30 years after the establishment of the International Pancreas Transplant Registry, more than 48 000 simultaneous pancreas and kidney (SPK) transplant cases were completed [1]. Throughout the years, preference has moved away from the systemic-bladder drainage technique and toward the systemic enteric drainage technique [1]. With a shift toward different surgical techniques, the complications associated with SPK have also changed. Gastrointestinal (GI) bleeds are one of the most common complications associated with SPK; however, most of these hemorrhages are associated with ulcers at the duodenojejunostomy anastomosis and also associated with cytomegalovirus (CMV) infection [2]. Due to the location of this anastomosis, endoscopy is usually not effective in the diagnosis or treatment of these ulcers [1]. This case report describes a postoperative GI hemorrhage after an SPK with a jejunal ulcer found distal to the anastomosis and treated using push endoscopy technique.
CASE REPORT
A 48-year-old male with type I diabetes and hypertension complicated by end-stage renal disease requiring dialysis for 1 year underwent an SPK transplant. The pancreas transplant was performed using the entero-systemic drainage technique as a hand-sewn side-to-side anastomosis between the donor duodenum and the recipient mid-jejunum, ~150 cm away from the ligament of Tritez with two layers. The patient initially progressed well through his operative course as expected. He had adequate blood glucose control without exogenous insulin, and adequate urine output and normal creatinine. Prior to discharge, he started to develop hematochezia that required blood transfusion.
The Department of Gastroenterology was consulted to performing an esophago-gastro-duodenoscopy to rule out upper GI bleeding, which noted a normal esophagus, stomach and duodenum. However, the endoscopic exam indicated bright red blood refluxing from the jejunum. A push enteroscopy technique was utilized by the gastroenterologist, who was able to visualize the duodenojejunostomy anastomosis and find the bleeding jejunum ulcer proximal to the anastomosis with an adherent clot near the site of anastomosis (Fig. 1). The area was washed out and injected with 6 ml of 1:10 000 solution of epinephrine for hemostasis and two GI clips were placed. Post-procedure, his hemoglobin stabilized, and within 2 days, he was able to be discharged home.
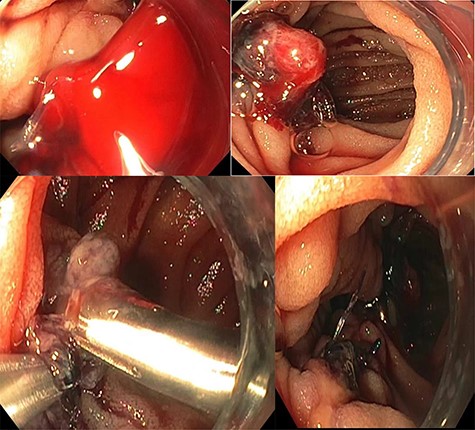
The bleeding jejunum ulcer proximal to the anastomosis with an adherent clot near the site of anastomosis.
DISCUSSION
More than 48 000 pancreas transplants were performed in the first 30 years after the establishment of the International Pancreas Transplant Registry. [1] Despite the high volume, pancreas transplants continue to have high complication rates, many of which resulted in subsequent early posttransplant graft loss [2]. The nature of these complications is directly related to variations in the surgical technique throughout the continued elaboration of pancreas transplants.
Initially, the most common technique in transplantation was a systemic-bladder technique. This approach allowed for easy monitoring of graft function via urinary amylase and cystoscopy [2], such as recurrent urinary tract infections, metabolic acidosis, reflux pancreatitis, hematuria, urethritis and urethral strictures [3]. As these patients were converted to the enteric drainage technique, the popularity of the duodenojejunostomy for enteric drainage began to rise.
Today, this surgical approach is most commonly used but is associated with a new category of surgical complications [2]. GI bleeding is a common complication identified postoperatively [3]. These may present in the immediate postoperative period or years later. Distant GI bleeds have been associated with pancreatic-aortic fistulas and pseudoaneurysm rupture [4, 5]. Reports of ulcers related to CMV infection have also been reported [2]. In the immediate postoperative period, GI bleeding has been associated with an ulcer at the duodenal stump and recipient jejunum anastomosis [2].
While studies have shown that these hemorrhages have only a small impact on outcome and graft survival, these hemorrhages, as described above, can be life-threatening. Given that most enteric anastomoses are established in the middle third of the GI tract, standard endoscopy is not applicable [1].
This case study brings two unique aspects of postoperative GI bleeding after SPK. First, the ulcer identified as the source of bleeding was proximal to the anastomosis in the jejunum. Second, the ability to use push endoscopy to identify and treat the ulcer is not described in the literature currently. One of the limitations of an entero-enteral anastomosis, such as duodenojejunostomy, is that endoscopy cannot be readily used to visualize the transplanted organ as previously done via cystoscopy. However, the use of push endoscopy may prove to be a less invasive intervention for GI bleeding after SPK.
GI bleeding is a common postoperative complication after an SPK transplant. Many times, these hemorrhages occur at the duodenojejunostomy due to reduced blood flow to the graft or due to CMV related ulcers at the anastomosis. This case study describes a hemorrhage from a bleeding ulcer, not near the anastomosis, and describes the use of the push enterorrhaphy technique to be both diagnostic and therapeutic.
CONFLICT OF INTEREST STATEMENT
None declared.



