-
PDF
- Split View
-
Views
-
Cite
Cite
Esubalew Taddese Mindaye, Dereje Giduma, Tesfaye H Tufa, Obturator hernia: case report, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa389, https://doi.org/10.1093/jscr/rjaa389
Close - Share Icon Share
Abstract
Obturator hernia, protrusion of abdominal content through the obturator foramen, is a rare type of abdominal wall hernia. Late patient presentation is associated with significant morbidity and mortality. We present rare case of obturator hernia causing small bowel obstruction in a 65-year-old-female patient. She presented with crampy abdominal pain, nausea and vomiting of three days duration. She was diagnosed with acute surgical abdomen and managed surgically at Arsi University College of health sciences, Assela, Ethiopia. Intraoperative finding revealed left-side obturator hernia, which is an extremely rare occurrence. Despite delayed presentation, our patient had smooth postoperative recovery. Obturator hernia is exceedingly rare, and it poses a diagnostic challenge as signs and symptoms are often nonspecific, making a preoperative diagnosis difficult. So, it should be considered as differential diagnosis in elderly patients presenting with acute surgical abdomen.
INTRODUCTION
Although it accounts for only 1% of all abdominal wall hernias, obturator hernia has relatively higher morbidity and mortality (15–25%), mainly due to delayed diagnosis with infarcted bowel (60–75%) [1, 2]. It was first described by Pierre Roland Arnaud de Ronsil in 1724 as a rare type of pelvic hernia [3]. The typical patients are elderly, multiparous, chronically ill and thin women being named as ‘the skinny old lady hernia’ [2, 4–6]. This is because women have broader pelvis and larger obturator canal [6]. In emaciated elderly people, loss of fatty tissue coupled with increased intraabdominal pressure facilitates the hernia formation [6, 7]. Obturator hernia commonly occurs on the right side due to larger sigmoid on the left side protecting the canal [6].
Accurate pre-operative diagnosis of obturator hernia is usually difficult, and most patients are operated as intestinal obstruction of unknown cause [8]. Patient presentations are nonspecific ranging from thigh or knee pain in the affected side to recurrent bouts of intestinal obstruction with cramping abdominal pain, nausea and vomiting [7, 8]. Howship–Romberg sign, which refers to ipsilateral groin pain aggravated by extension, abduction and medial rotation, radiating down the thigh as a result of irritation of the obturator nerve, is a characteristic sign of obturator hernia. However, it is present in only 15–50% of the patients with obturator hernia [2, 5, 8].
Plain radiographs often show nonspecific findings of small bowel obstruction and are seldom helpful in diagnosing obturator hernia [9]. Ultrasonography is also useful and reliable in the diagnosis of obturator hernia [10], but it is often limited by the relative inaccessibility of this deep region and is operator dependent. A computed tomography scan can accurately diagnose not only an obturator hernia but also other conditions of bowel obstruction [2, 9].
Surgical management through midline abdominal incision is preferred for an obturator hernia, as it gives adequate exposure, allows reduction of hernia content and facilitates bowel resection if necessary [9].
CASE PRESENTATION
Sixty-five-year-old-female patient with known cardiac illness on follow-up for the last 10 years presented with crampy central abdominal pain associated with nausea, frequent bilious vomiting of 3 days duration. She has no previous experience of similar compliant and has no previous abdominal surgery. For the above compliant, she went to nearby clinic from where she was referred to Assela referral hospital for better evaluation and management. On arrival to emergency surgical department, she was emaciated, acutely sick looking with tachycardia of 110 beat/minutes and blood pressure of 130/75mmhg. Abdominal examination revealed distended, hypertympanic abdomen with hyperactive bowel sound, but there was no sign of peritoneal irritation. Hernial sites were free, and digital rectal examination was unremarkable. Nasogastric tube insertion revealed bilious gastrointestinal content, and her basic laboratory examinations showed leukocytosis of 12,000 with left shift (neutrophil 85%), while plain abdominal X ray (Fig. 1) showed dilated small bowel loops with absent rectal gas shadow.

Plain abdominal X-ray showing dilated small bowel loops with visible valvulae conniventes.
With the diagnosis of acute abdomen secondary to small bowel obstruction, she was prepared and operated through midline abdominal incision. Intraoperatively, there was herniated anti-mesenteric side of ileum about 20 cm proximal to ileocecal valve through the left obturator foramen (Richter type) (Fig. 2). The bowel proximal to the hernia was dilated, while the distal segment was collapsed. Upon reduction, the hernia content was viable. The orifice of the obturator canal was closed with simple interrupted silk sutures, and laparotomy incision was closed in layers. Subsequently, the patient showed a remarkable improvement and was discharged from the hospital in a stable condition after 4 days of stay. Her follow-up for 6 months following surgery showed a normal post-operative course, and the patient was happy with her treatment.
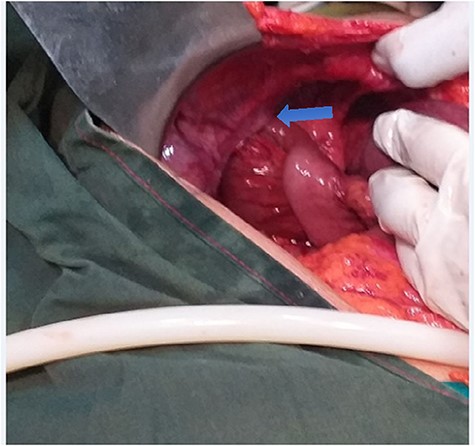
Intraoperative picture showing herniated small bowel through the left obturator foramen.
DISCUSSION
Obturator canal is an opening in the superolateral part of the obturator foramen containing the obturator nerve and vessels. It is 2–3 cm long and 1 cm wide, and is usually filled with fat, allowing no space for hernia [2]. Loss of body fat and increase in intra-abdominal pressure are the major factors that lead to the development of hernia [2, 5]. Weakened pelvic floor with multiple pregnancy, older age and emaciation due to her chronic illness are contributing factors in our patient. The commonest content of the sac is ileum with about 50% being of the Richter’s type, and our patient fits to this common type [2]. The most common clinical presentation is intestinal obstruction of an unknown cause as has occurred in our patient [2, 8]. Although abdominopelvic CT scan is sensitive to diagnose obturator hernia preoperatively [2], most patients’ diagnosis are reached intraoperatively like our patient as it is an uncommon cause of acute surgical abdomen. Unlike the common finding in literatures, this patient has left obturator hernia, which is extremely a rare occurrence.
Mainstay of treatment is surgery [4]. The approach can be via transperitoneal approach (lower midline laparotomy), abdominal extraperitoneal approach or laparoscopically [8]. Lower midline laparotomy is the most common surgical approach in emergency cases as it gives the best exposure, allows reduction of hernia content and facilitates bowel resection if necessary [6, 9]. The hernia repair can be a simple closure of the entrance of the canal with interrupted sutures or repair with mesh [5].
Patients with advanced age, associated respiratory and cardiovascular diseases and with late diagnosis have higher mortality rate up to 70% [5, 8]. Although our patient fulfills some of these risks, she had smooth recovery likely due to absence of bowel infarction.
CONCLUSION
Obturator hernia as a cause of bowel obstruction is one of the rare surgical phenomenon. Preoperative diagnosis of obturator hernia is challenging due to nonspecific presentation and usually made intraoperatively. Delay in diagnosis, medical comorbidity and old age are associated with poor outcome. Despite having delayed presentation, our patient has good postoperative outcome.
CONFLICT OF INTEREST STATEMENT
None declared.
AUTHORS' CONTRIBUTIONS
E.M. was involved in the surgery, conceived and conducted the study, did literature search and critical revision of the manuscript. D.G. was involved in the surgery, over all supervision of the manuscript and critical revision of the manuscript, T.T. did the overall supervision of the manuscript and critical revision of the manuscript. All authors have read and approved the manuscript.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images.



