-
PDF
- Split View
-
Views
-
Cite
Cite
Ana V M Faustino, Tiago F Rama, Margarida P C Andrade, Vítor M D Carneiro, Maria I G P Leite, A rare tumour, a singular indication: sleeve gastrectomy in a morbidly obese septuagenarian with gastric schwannoma, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa421, https://doi.org/10.1093/jscr/rjaa421
Close - Share Icon Share
Abstract
Gastric schwannoma is an extremely rare mesenchymal tumour, representing only 0.2% of all gastric tumours. Obesity is an alarming worldwide disease whose only effective and sustained treatment seems to be surgical. We present a case of a 73-year-old female with epigastric pain and unspecific dyspeptic symptoms, whose diagnostic endoscopic procedures raised suspicion of a gastrointestinal stromal tumour. Given her good performance status, and since grade 2 obesity with high-risk comorbid conditions was present, she was considered a suitable candidate for laparoscopic sleeve gastrectomy. Both surgery and immediate postoperative period were uneventful. Histological and immunocytochemical analysis classified the tumour as benign gastric schwannoma. After 24 months, besides being disease-free, she presented an excess weight loss of 90.2%, with improvements in metabolic profile allowing withdrawal from chronic medication. The patient is healthier, satisfied and living an active life, showing that age by itself should not be a deterrent to bariatric surgery.
INTRODUCTION
Gastrointestinal mesenchymal tumours arise from mesenchymal stem cells and embrace a heterogeneous group of spindle cell tumours including gastrointestinal stromal tumour (GIST), leiomyoma, leiomyosarcoma and schwannoma [1].
GIST is the commonest of mesenchymal tumours, generally located in the stomach (60–70%) [2] with a malignancy transformation rate of 10–30% [1–3].
Gastric schwannoma is extremely rare, representing only 0.2% of all gastric tumours, 4% of the benign ones [2–4]. Patients are frequently asymptomatic, but may present upper gastrointestinal bleeding, epigastric pain or a palpable epigastric mass [4]. Malignant transformation has already been described, but is extremely rare [3], hence, prognosis is excellent after complete surgical resection [4].
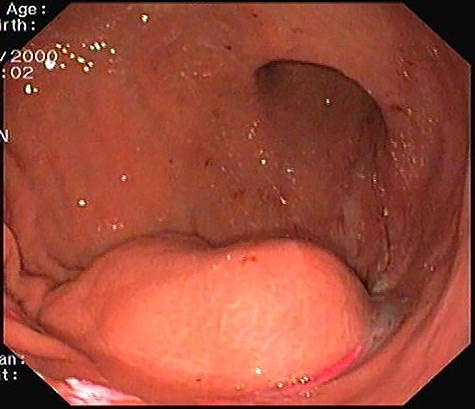
Upper gastrointestinal endoscopy: 4 cm subepithelial lesion located at gastric antrum.
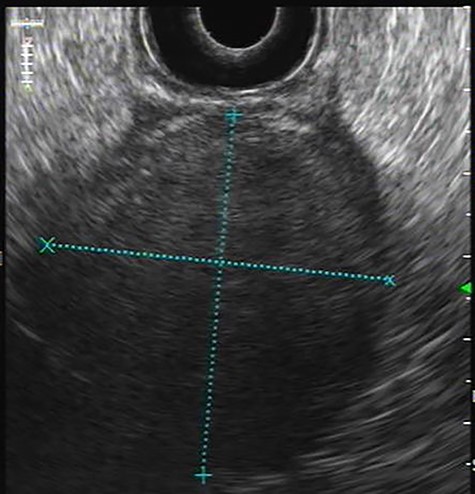
Endoscopic ultrasonography: Hypoechoic homogeneous lesion, growing on the 4th layer of gastric wall with regular contours, well-defined limits and negative Doppler sign; no cystic aspects were found; gastrointestinal stromal tumour diagnosis was suggested.

Computed tomography contrast-enhanced scan: predominantly exophytic neoplasm growing from gastric greater curvature (arrow) with 97 × 77 × 57 mm; no signs of metastatic or locally advanced disease were found.

Surgical specimen, gastric schwannoma: intramural, nodular, solid mass measuring 85 × 60 × 60 mm. A cross-section revealed a yellowish homogeneous tumour, well-delimited though not capsulated.
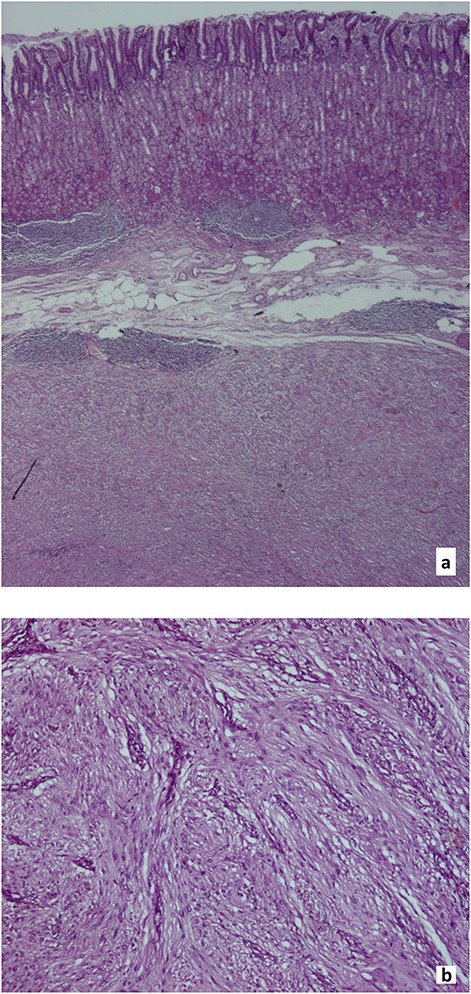
Histological findings, gastric schwannoma: a. Muscularis propria tumour, surrounded by peripheral lymphoid aggregates (Hematoxylin and eosin, x20). b. Spindle cells with palisading nuclei, arranged in a fascicular pattern with rare mitosis (1/30 high-power field) and no necrosis (Hematoxylin and eosin, x100).
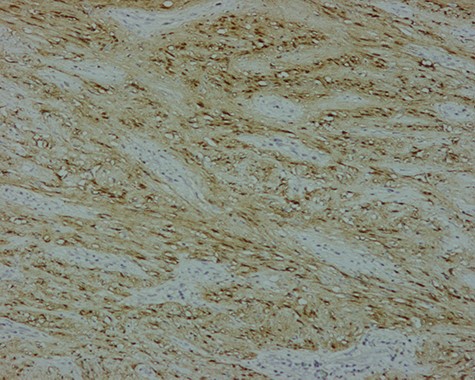
Immunohistochemistry, gastric schwannoma: Tumour cells with strongly positive nuclear staining for S-100 (S-100, x100).
Obesity is a worldwide and all age group affecting disease. Improvements in surgical and medical skills have led to better outcomes regardless of the patients’ age group, and yet performing bariatric surgical procedures in elderly patients still is a controversial subject [5, 6].
The term ‘morbid obesity’ is reserved to define patients with a body mass index (BMI) ≥ 40.0 kg/m2 or with a BMI between 35.0 and 39.9 kg/m2 plus obesity-related comorbidities, such as diabetes, hypertension, dyslipidaemia, among others [7, 8].
CASE REPORT
We report a case of a 73-year-old morbidly obese female, with a 38.84 kg/m2 BMI under lipid-lowering drugs and three different classes of antihypertensive drugs.
Presenting an initial clinical picture of epigastric pain and nonspecific dyspeptic symptoms, the patient underwent upper gastrointestinal endoscopy (Fig. 1) where a subepithelial lesion was found, mandating further investigation. Endoscopic ultrasonography (Fig. 2) arose suspicion of GIST and computed tomography scan (Fig. 3) revealed an exophytic lesion with 97 × 77 × 57 mm rising from the gastric greater curvature, with no signs of metastatic or locally advanced disease.
Considering the tumour’s location and the presence of grade 2 obesity with cardiovascular risk factors, a multidisciplinary group meeting proposed laparoscopic sleeve gastrectomy and informed consent was obtained. Both peri and postoperative periods were uneventful, patient was discharged after 5 days.
Inspection of surgical specimen (Fig. 4) showed an intramural, nodular, solid mass measuring 85 × 60 × 60mm with unremarkable overlaying mucosa; a cut section revealed a yellowish homogeneous tumour. Histological examination (Fig. 5) revealed a well-delimited, but not capsulated mass, centred at muscularis propria, surrounded by peripheral lymphoid aggregates. Spindle cells with palisading nuclei, arranged in a fascicular pattern, slight pleomorphic, rare mitosis (1/30 high-power field) and no necrosis characterized this tumour. Resection margins were negative for tumour cells. Additionally, immunohistochemistry of tumour cells showed strongly positive nuclear staining for S-100 (Fig. 6) and SOX10, consistent with the diagnosis of benign schwannoma.
After 6 months of surgery the patient had no gastrointestinal complaints and showed an excess weight loss (EWL) of 53.5% with a BMI of 31.43 kg/m2. Furthermore, a reduction in the need of chronic medication was achieved, with optimal blood pressure profile under antihypertensive monotherapy and sustained normal range cholesterol and triglycerides values without administration of targeted therapy (Tables 1 and 2). An EWL of 90.2% was noted 24 months after the surgery, translating into a thankful patient living an active life with a BMI of 26.35 kg/m2.
| Standardized outcomes . | Preop . | 6 Months postop . | 24 Months postop . |
|---|---|---|---|
| Height | 1.63 | – | – |
| Weight | 103.2 | 83.5 | 70.0 |
| EW | 36.8 | 17.1 | 3.6 |
| BMI | 38.84 | 31.43 | 26.35 |
| Δ BMI | – | 7.41 | 12.49 |
| TWL | – | 19.7 | 33.2 |
| %TWL | – | 19.1 | 32.2 |
| %EBMIL | – | 53.5 | 90.4 |
| %EWL | – | 53.5 | 90.2 |
| Standardized outcomes . | Preop . | 6 Months postop . | 24 Months postop . |
|---|---|---|---|
| Height | 1.63 | – | – |
| Weight | 103.2 | 83.5 | 70.0 |
| EW | 36.8 | 17.1 | 3.6 |
| BMI | 38.84 | 31.43 | 26.35 |
| Δ BMI | – | 7.41 | 12.49 |
| TWL | – | 19.7 | 33.2 |
| %TWL | – | 19.1 | 32.2 |
| %EBMIL | – | 53.5 | 90.4 |
| %EWL | – | 53.5 | 90.2 |
EW, excess weight (kg); BMI, body mass index (kg/m2); Δ BMI, change in BMI (kg/m2); TWL, total weight loss (kg); %TWL, percent of total weight loss; %EBMIL, percent of excess BMI loss; %EWL, percent of EWL.
| Standardized outcomes . | Preop . | 6 Months postop . | 24 Months postop . |
|---|---|---|---|
| Height | 1.63 | – | – |
| Weight | 103.2 | 83.5 | 70.0 |
| EW | 36.8 | 17.1 | 3.6 |
| BMI | 38.84 | 31.43 | 26.35 |
| Δ BMI | – | 7.41 | 12.49 |
| TWL | – | 19.7 | 33.2 |
| %TWL | – | 19.1 | 32.2 |
| %EBMIL | – | 53.5 | 90.4 |
| %EWL | – | 53.5 | 90.2 |
| Standardized outcomes . | Preop . | 6 Months postop . | 24 Months postop . |
|---|---|---|---|
| Height | 1.63 | – | – |
| Weight | 103.2 | 83.5 | 70.0 |
| EW | 36.8 | 17.1 | 3.6 |
| BMI | 38.84 | 31.43 | 26.35 |
| Δ BMI | – | 7.41 | 12.49 |
| TWL | – | 19.7 | 33.2 |
| %TWL | – | 19.1 | 32.2 |
| %EBMIL | – | 53.5 | 90.4 |
| %EWL | – | 53.5 | 90.2 |
EW, excess weight (kg); BMI, body mass index (kg/m2); Δ BMI, change in BMI (kg/m2); TWL, total weight loss (kg); %TWL, percent of total weight loss; %EBMIL, percent of excess BMI loss; %EWL, percent of EWL.
| Laboratory data . | Preop . | 6 Months postop . | 24 Months postop . |
|---|---|---|---|
| Haemoglobin, g/dl (12–15.5) | 13.3 | 12.5 | 12.2 |
| Albumin, g/dl (3.4–5.0) | 4.1 | 3.6 | 4.1 |
| Blood glycose, mg/dl (<100) | 105 | 91 | 89 |
| Total cholesterol, mg/dl (<200) | 169 | 175 | 201 |
| HDL, mg/dl (>40) | - | 50 | 61 |
| LDL, mg/dl (<100) | - | 108 | 132 |
| Triglycerides, mg/dl (<150) | 130 | 101 | 103 |
| Laboratory data . | Preop . | 6 Months postop . | 24 Months postop . |
|---|---|---|---|
| Haemoglobin, g/dl (12–15.5) | 13.3 | 12.5 | 12.2 |
| Albumin, g/dl (3.4–5.0) | 4.1 | 3.6 | 4.1 |
| Blood glycose, mg/dl (<100) | 105 | 91 | 89 |
| Total cholesterol, mg/dl (<200) | 169 | 175 | 201 |
| HDL, mg/dl (>40) | - | 50 | 61 |
| LDL, mg/dl (<100) | - | 108 | 132 |
| Triglycerides, mg/dl (<150) | 130 | 101 | 103 |
HDL, high density lipoprotein cholesterol; LDL, low density lipoprotein cholesterol.
| Laboratory data . | Preop . | 6 Months postop . | 24 Months postop . |
|---|---|---|---|
| Haemoglobin, g/dl (12–15.5) | 13.3 | 12.5 | 12.2 |
| Albumin, g/dl (3.4–5.0) | 4.1 | 3.6 | 4.1 |
| Blood glycose, mg/dl (<100) | 105 | 91 | 89 |
| Total cholesterol, mg/dl (<200) | 169 | 175 | 201 |
| HDL, mg/dl (>40) | - | 50 | 61 |
| LDL, mg/dl (<100) | - | 108 | 132 |
| Triglycerides, mg/dl (<150) | 130 | 101 | 103 |
| Laboratory data . | Preop . | 6 Months postop . | 24 Months postop . |
|---|---|---|---|
| Haemoglobin, g/dl (12–15.5) | 13.3 | 12.5 | 12.2 |
| Albumin, g/dl (3.4–5.0) | 4.1 | 3.6 | 4.1 |
| Blood glycose, mg/dl (<100) | 105 | 91 | 89 |
| Total cholesterol, mg/dl (<200) | 169 | 175 | 201 |
| HDL, mg/dl (>40) | - | 50 | 61 |
| LDL, mg/dl (<100) | - | 108 | 132 |
| Triglycerides, mg/dl (<150) | 130 | 101 | 103 |
HDL, high density lipoprotein cholesterol; LDL, low density lipoprotein cholesterol.
DISCUSSION
Gastric schwannoma and GIST are both mesenchymal tumours, sharing features as age incidence, clinical and radiological characteristics and gross morphology [2–4]. Therefore, even with the latest imaging technology, getting a precise diagnosis before a surgical procedure may prove difficult or even impossible. Definitive diagnosis can only be established through histopathological and immunohistochemical examination of the surgical specimen [4].
While GIST is the commonest mesenchymal tumour, schwannoma is extremely rare, especially in gastrointestinal tract. Gastric schwannoma is a slow-growing tumour from Schwann cell sheaths that frequently grow intramurally (65%) at gastric body (50%), affecting predominantly females in their 5th to 6th decades of life [4].
Prognosis is excellent after complete surgical resection given schwannoma’s rare malignancy transformation rate [1, 2, 4].
Regarding obesity, a debilitating, lifelong metabolic worldwide disease, studies have been pointing surgery as the most impactful treatment in terms of weight loss, comorbidities, quality of life and life expectancy [7, 8].
High mortality rates and other previously undesired outcomes in patients over 50 years of age have contributed to a certain stigma towards the role of bariatric surgery in elderly patients [5].
Actual guidelines consider surgery for morbidly obese patients aged 18–60 years [7, 8], however, as the population ages and life expectancy increases, we have been witnessing raising numbers of elderly obesity [9], making its management, in terms of comorbidities and quality of life, a public health matter.
Due to a refinement in preoperative care, increased surgical experience, improved materials and better knowledge of bariatric medicine, weight loss surgical procedures have been proving to be safe and effective even in older patients, disregarding age as an absolute contraindication [5, 6].
Despite this improvement, this issue remains somewhat controversial [5], beginning by the proper definition of ‘elderly patients’ since it varies according to different trials from over 50 to over 70 years of age [9]. Furthermore, data based on long-term follow-up are still lacking.
Laparoscopic sleeve gastrectomy was initially used as a first-stage procedure mainly in high-risk patients—to reduce weight, comorbidities and operative risk—, but thanks to its relative technical simplicity, reliability and lesser risk compared with other bariatric surgical procedures [9], it has been used as the main weight loss procedure in this age group [6, 8].
Complications of sleeve gastrectomy include early leakage along the staple line and long-term weight regain due to expansion of the sleeve. On the other hand, improvements in diabetes, hypertension, dyslipidaemia and sleep apnoea are seen in nearly all patients [8], including ours.
A multidisciplinary approach allows the best preoperative evaluation and optimization and guarantees appropriate postoperative care, making it a standard practice among morbidly obese patients [6].
To our knowledge, this is the first case report of a surgical intervention in which a gastric schwannoma resection was performed concomitantly with a bariatric procedure in an over 70-year-old patient, with remarkable outcomes according to standard [10]. Nevertheless, a rigorous longer-term follow-up should be performed with special focus on preventing the development of nutritional deficiencies.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
ETHICAL APPROVAL
Written informed consent from patient to publish the case and images.



