-
PDF
- Split View
-
Views
-
Cite
Cite
Joseph Yorke, Francis Akwaw Yamoah, Ronald Awoonor-Williams, Thomas Okpoti Konney, Emmanuel Acheampong, Ernest Adjei, Kwabena Acheamfour Ababio, Daniel Gyawu Aning, Dennis Afful-Yorke, Freda Manu Aidoo, Claudia Gyamfua Assim, Frank Enoch Gyamfi, Raphael Owusu Sekyere Assim, Saabea Owusu Konadu, David Elikplim Kuwornu, Emmanuella Nsenbah Acheampong, Familial adenomatous polyposis: a case study, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa367, https://doi.org/10.1093/jscr/rjaa367
Close - Share Icon Share
Abstract
Familial adenomatous polyposis (FAP) is an inherited syndrome characterized by several adenomatous polyps of the gastrointestinal (GI) mucosa. If treatment is not provided, an average individual with classic FAP will develop colorectal carcinoma around the age of 40 years. The incidence rate of FAP in developing countries like Ghana is unknown compared to advanced countries. We present the first FAP case of a 22-year-old Ghanaian female who presented with massive lower GI bleeding and underwent surgical management after a thorough investigation. The initial assumption that colonic polyps are scarce in native Africans may be more than what is perceived. This highlights the need for the availability of endoscopic services in Ghana.
INTRODUCTION
Familial adenomatous polyposis (FAP) is an inherited syndrome characterized by several adenomatous polyps of the gastrointestinal (GI) mucosa [1]. The incidence of FAP is ~1 in 7000 to 1 in 30 000 births [2]. Generally, the number of GI polyps correlates with increasing age. The presentation is usually asymptomatic in the majority but may present with diarrhoea, bleeding per rectum and abdominal pain, tenesmus, and obstruction from the second to the third decade of life [3].
We present a 22-year-old female with FAP who presented with massive lower GI bleeding and underwent surgical management after a thorough investigation.

CASE Report
A 22-year-old female graduate engineer presented to the accident and emergency unit with recurrent episodes of bleeding per rectum for the past 2 years which was bright red, devoid of stools and associated abdominal pain. The index presentation at the accident and emergency unit was severe with about five (5) episodes associated with dizziness, palpitations, and easy fatigability. Significantly, she had lost weight and had not noticed any protrusion of mass from the anus on defecation or had any history of epigastric pain or haematemesis.
On examination, she had signs of blood pressure of 80/40 mmHg and a pulse of 120 beats per minute. Abdominal examination was unremarkable. On digital rectal examination, haemorrhoids were felt and the examining finger was however stained with bright red blood. She was resuscitated with crystalloids and blood products. Initial Hb on presentation was 4.3 g/dL.
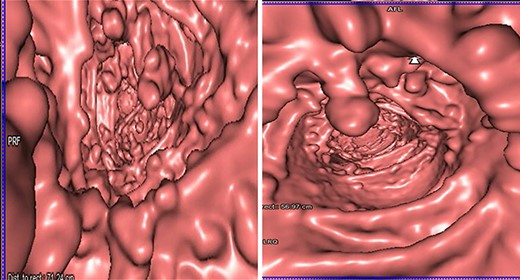
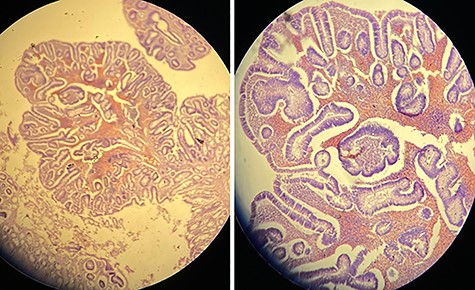
Colonoscopy up to the sigmoid colon done showed external haemorrhoids, numerous polyps of varying sizes throughout the rectum and sigmoid colon from which biopsies were taken (Fig. 1). The rectal polyps were few (Fig. 1). Histology showing low-grade dysplastic epithelium comprised of hyperchromatic and elongated nuclei arranged in a pseudostratified manner (Fig. 2). Features consistent with tubular adenoma with low-grade intraepithelial neoplasia (Fig. 2). However, a carcino-embryonic antigen test done at the time was 12.4 μg/L.
A computed tomography (CT) virtual colonoscopy was done to complete the picture which detailed the extent of the polyps (Fig. 3). Thousands of polyps filling the entire colon with relative sparing of the caecal region and the proximal part of the ascending colon covering a length of ~15 cm (Fig. 3). With sizes ranging from millimetres to the largest measuring ~2.6 cm.
Photomicrographs of large bowel showing polypoid lesions (H and E, x40).
The patient was optimized for surgical intervention with more blood products followed by laparotomy with subtotal colectomy (with bowel length of 62 cm) and ileorectal anastomosis. Intra-op multiple polyps spanning the entire colon was seen. Histopathology report of the colonic specimen revealed mucosal surface with a myriad of multiple raised lesions (>1000). The smallest had an average size of 0.5 × 0.5 cm. In some areas, the lesion appeared in aggregate with areas of mucosal ulceration. Seven lymph nodes were retrieved from the attached mesentery. Microscopically, multiple adenomatous polyps with mild dysplasia were seen. There were no high-grade changes. The section from the appendix shows lymphoid hyperplasia with reactive follicles. There was no malignancy or severe dysplasia. However, features were consistent with Adenomatous Polyposis Coli.
Fourteen days post-op, the patient has shown marked improvement in recovery with Hb of 12.9 g/dL and carcino-embryonic antigen test was 2.1 μg/L. The patient was placed on a high-fibre diet and is currently doing well.
DISCUSSION
FAP has been described as rare in native Africans [4]. However, emerging studies on colonoscopy results within the sub-region show a rising number of cases of colonic polyps with these lesions having low malignant potential from the histological analysis [5]. The index case had been in and out of the hospital with a recurrent episode of peri-rectal (PR) bleeding and manage as dysentry. This underscores the need to have a high index of suspicion in our population especially in the wake of the emerging data.
Massive lower GI bleeding with attendant class four shock from FAP is a rare occurrence as well as requiring urgent surgical intervention after investigation with Oviedo et al. reporting of such a case in an African American male [6]. Four cases have been previously reported in a Nigerian population [7], but this is the first of its kind in a Ghanaian population to the best of our knowledge.
The standard surgical options for management of FAP include total proctocolectomy with Brookes ileostomy or ileal pouch with ileoanal anastomosis and subtotal colectomy with ileorectal anastomosis [8]. The option for subtotal colectomy with ileorectal anastomosis was based on the few polyps noted on the colonoscopy in the rectum. It has been documented that the risk of developing cancer in the residual rectum ranges from 13 to 59% by 25 years [9]. However, it avoids the need for a permanent ileostomy which the index case was not desirous and is willing to undergo regular surveillance for residual rectum which is mandatory in this category of patients. Furthermore, in women of childbearing age with a low burden of polyps in the rectum, it is a more acceptable option in the preservation of fertility than the ileoanal anastomosis with a pouch [10]. Due to the unavailability of the needed screening tools in our facility, genetic testing was not conducted in this patient and high-risk family members.
CONCLUSION
The initial assumption that colonic polyps are scarce in native Africans may be more than what is perceived. This highlights the need to make endoscopic services available particularly in young patients presenting with lower GI bleeding.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



