-
PDF
- Split View
-
Views
-
Cite
Cite
Benjamin D Tift, Joshua T Prickett, Lorenzo K Sampson, Scalp mass: an atypical presentation of multiple myeloma, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa410, https://doi.org/10.1093/jscr/rjaa410
Close - Share Icon Share
Abstract
A 64-year-old male with no history of trauma presented to the general surgery clinic with a 6-month history of an asymptomatic left parietal scalp mass. The differential included benign etiologies such as lipoma or sebaceous cyst. At surgery, a hemorrhagic soft tissue mass with underlying defect in the parietal calvarium was noted. The initial attempt at resection was abandoned and neurosurgical consultation was requested. Magnetic resonance imaging demonstrated an enhancing scalp mass with a lytic lesion of the parietal calvarium with no intradural extension. Craniectomy with mass resection and mesh cranioplasty were performed. Pathology confirmed plasma cell neoplasm; serum protein electrophoresis and lytic skull lesions confirmed multiple myeloma. This rare presentation of multiple myeloma serves as a call for providers to maintain a broad differential when evaluating a seemingly benign mass, consider rare etiologies when appropriate and maintain vigilance for abnormal findings during any procedure.
INTRODUCTION
Multiple myeloma is a plasma cell malignancy with variable presentations. Some present with nonspecific symptoms, including bone pain, fatigue, weakness and weight loss. Others will be asymptomatic but present with laboratory abnormalities including anemia, hypercalcemia and renal insufficiency. Multiple myeloma diagnostic criteria include presence of end organ damage and either clonal bone marrow plasma cells >10% or a biopsy-proven bony tumor or extramedullary plasmacytoma [1]. Here we discuss a previously healthy 64-year-old male with a scalp mass as the initial and sole presenting finding of multiple myeloma.
CASE REPORT
A 64-year-old male presented to the general surgery clinic with a 6-month history of a gradually enlarging scalp mass. He recently experienced paresthesia in the region but no pain, drainage or redness. Medical and surgical history includes appendectomy, laparoscopic cholecystectomy, cystourethroscopy with stone excision, anxiety and hypercholesterolemia, with no current medications. He denied tobacco or illicit drug use and consumed little alcohol. He denied weight loss, fever, chills, weakness, fatigue, vision disturbance, recurrent infections or head trauma. Physical exam was normal, except for a 4-cm fluctuant, mobile mass over the left parietal bone.
The initial differential included benign causes of scalp masses, such as lipoma, epidermoid cyst, sebaceous cyst, abscess or hematoma. In the office, the patient was consented for mass aspiration. No fluid was obtained, increasing suspicion for a solid mass. Excision was scheduled at the outpatient surgical center.
Under general anesthesia, a linear incision was made over the parietal scalp mass. Upon dissection, soft hemorrhagic tissue was encountered, with a defect extending through the left parietal bone and into the cranial cavity. The cavity was packed with hemostatic materials and the skin was closed. The patient was transferred to the emergency room for imaging and neurosurgery consultation.
Noncontrast head computed tomography (CT) confirmed a left parietal bone lytic lesion (Fig. 1). Brain magnetic resonance imaging (MRI) confirmed an enhancing mass involving the left lateral scalp and parietal bone extending down to the dura (Fig. 2). T1-weighted image noted additional small enhancing lesions of the frontal calvarium. Initial laboratory studies noted hypercalcemia (serum calcium 10.6 mg/dl) and anemia (hemoglobin 11.5 g/dl).

Head CT without contrast (coronal plane) showing a 3.3-cm lytic lesion of the left parietal calvarium with extension of soft tissue hyperdensity to the dural surface.
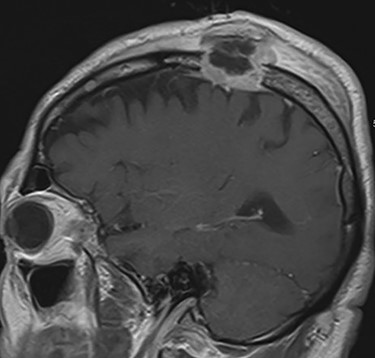
MRI brain T1 postcontrast view (sagittal plane) showing an avidly enhancing mass eroding through the left parietal bone and extending deep to the dura with scalp edema and thickening, in addition to smaller enhancing lesions of the frontal calvarium.
The differential diagnosis was expanded to include multiple myeloma, solitary plasmacytoma and metastatic disease. This presentation is consistent with the traditional diagnostic criteria of multiple myeloma, with bony lesions in the calvarium, hypercalcemia and anemia [1].
Neurosurgery recommended left parietal craniectomy, scalp mass resection and titanium mesh cranioplasty. Under general anesthesia the previous incision was opened and extended. A hemorrhagic soft tissue mass was noted, extending from the scalp to the dura. The mass was scraped off the dura, resected and noted to have not infiltrated intradurally. A circumferential craniectomy was performed surrounding the lytic defect. Several smaller areas of lytic bone adjacent to the lesion were drilled until normal bone was present at all edges. After achieving hemostasis, a titanium mesh plate was placed and secured. The wound was closed, the patient extubated and transferred to recovery. Scalp, bone and soft tissue specimens were sent to pathology. Postoperative CT head demonstrated mass resection without intracranial hemorrhage or complication.
Pathology determined the soft tissue mass to be of plasma cell origin (Fig. 3), with immunoreactivity for CD45, CD56, CD79a, CD138 and epithelial membrane antigen. In situ hybridization revealed kappa light chain expression. The excised parietal bone showed patchy, confluent intramedullary sheets of malignant plasma cells with hemorrhage and necrosis, confirming a plasma cell myeloma diagnosis (Fig. 4), and in conjunction with other smaller lytic lesions, a multiple myeloma diagnosis.
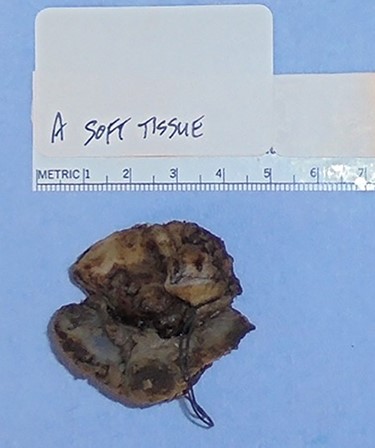
A 4.5-cm plasma cell myeloma made up of malignant plasma cells with large nucleoli positive for CD45, CD56, CD79a, CD138 and epithelial membrane antigen.
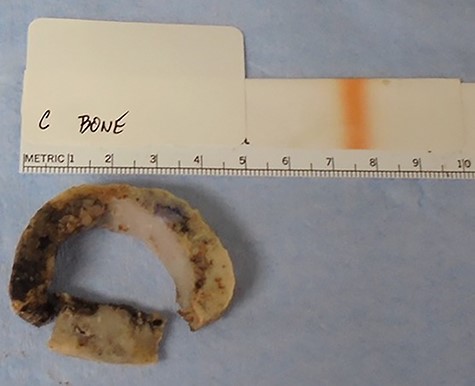
Excised portion of left parietal bone at the edge of the lytic lesion, containing patchy intramedullary sheets of malignant plasma cells with hemorrhage and necrosis.
Serum protein electrophoresis confirmed multiple myeloma with two M-spikes (1.6 g/dl and 0.4 g/dl), elevated serum-free kappa concentration (41.5 mg/l) and elevated kappa/lambda ratio (7.41). Peripheral blood smear noted rouleaux formation. Positron emission tomography/CT confirmed bony lesions throughout the axial (Fig. 5) and proximal appendicular skeleton. The patient is currently undergoing chemotherapy with autologous bone marrow transplant.

Positron emission tomography/CT showing numerous foci of uptake involving the axial skeleton (thoracic vertebral and rib lesions noted in this image).
DISCUSSION
The presentation of a minimally or asymptomatic scalp mass is a common scenario in the general surgery clinic. It is rare for a scalp mass to be the sole presenting symptom of multiple myeloma. Upon review of the literature, two cases where masses were the sole presenting symptom of multiple myeloma were found, and both were imaged before surgery [2, 3]. In one, the mass was painless and described as a ‘bony hard swelling’ [2], whereas the mass in our presentation was fluctuant. In the second case, the patient was completely asymptomatic, and MRI noted dura involvement, superior sagittal sinus invasion and cerebellar tonsil displacement [3]; in our presentation, the mass did not invade the dura or displace brain parenchyma. Although scalp masses have been noted on initial presentation of multiple myeloma, patients typically present with additional symptoms, including gait disturbance [4], acute weakness, bone pain and confusion [5]. There was also a case report of incidental discovery after imaging following head trauma [6]. Frequently, a scalp mass will be evaluated by a primary care clinician or general surgeon. In the absence of red flag historical or exam findings, it is common to proceed to excision or drainage without performing imaging or laboratory studies to rule out rare etiologies. Although preprocedure imaging was not indicated in this case and is not appropriate in most cases of minimally symptomatic scalp masses, providers must remain vigilant for unusual findings during the procedure. In this case a larger than expected amount of hemorrhage and a bony defect were noted.
Some may inquire about why an excision was performed versus initial biopsy. At the initial resection attempt, hemorrhage and a bony skull defect were encountered, raising suspicion of malignancy. Biopsy was not performed due to profuse bleeding. Hemostatic agent was applied with skin closure prior to transfer to a tertiary medical center with neurosurgical capabilities. Debulking was indicated given the wound was packed with hemostatic materials and needed hemostasis with definitive closure.
This rare presentation of a minimally symptomatic scalp mass as the sole presenting symptom of multiple myeloma serves as a call to providers to consider a wide differential when evaluating typically benign presentations, consider ruling out other etiologies with imaging and laboratories when appropriate and maintain vigilance for abnormal findings during any clinical procedure.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None declared.
References
- magnetic resonance imaging
- consultation
- lipoma
- epithelial cyst
- scalp
- cranium
- surgical mesh
- surgical procedures, operative
- wounds and injuries
- multiple myeloma
- neurosurgical procedures
- pathology
- protein electrophoresis, serum
- general surgery
- craniectomy
- calvaria
- lytic lesion
- atypical
- soft tissue mass



