-
PDF
- Split View
-
Views
-
Cite
Cite
Sylvie Bowden, Arash Jaberi, Graham Roche-Nagle, Large pseudoaneurysm arising from the deep femoral artery after hip fracture fixation, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa408, https://doi.org/10.1093/jscr/rjaa408
Close - Share Icon Share
Abstract
Hip fracture is a common condition of increasing global concern. Vascular injury as a complication after hip fracture repair is rare. A 90-year-old woman developed swelling and pain to her proximal thigh 1 month after uneventful hip fracture fixation. Ultrasound revealed a large pseudoaneurysm of the deep femoral artery, which was successfully treated with transcatheter embolization. Pseudoaneurysms have numerous etiologies. In this case, vascular injury is suspected to be a consequence of proximal migration of the lesser trochanteric fragment. Unfortunately, pseudoaneurysms are often not appreciated due to the nonspecific nature of the presenting symptoms. Diagnosis should be confirmed radiologically and management depends on the location and size of the pseudoaneurysm, as well as patient comorbidities. Pseudoaneurysm after hip fracture fixation is a rare but serious complication. Diagnosis is challenging due to nonspecific symptoms. A high index of suspicion is imperative to prevent life-threatening rupture.
INTRODUCTION
Hip fracture is a common clinical condition, with lifetime risk as high as 18% for females and 6% for males [1]. Risk factors can be grouped as those decreasing bone mineral density or increasing falls risk; thus, they are especially common among the elderly and of increasing global concern due to the aging population [2].
Vascular injury as a complication after hip fracture repair is rare, with reports ranging from 0.05 to 0.49% [3, 4]. Injury may be due to the trauma itself, during repair or less commonly postoperatively. Causes include direct injury by bony fragments and bony fragment migration [4, 5].
We present a case of deep femoral artery (DFA) pseudoaneurysm in a 90-year-old woman 1 month after uneventful hip fracture fixation.
CASE REPORT
A 90-year-old woman suffered a mechanical fall at home, immediately developed left hip pain and inability to weight-bear, and was brought to the emergency room. Radiographs revealed a displaced intertrochanteric hip fracture with a separate greater trochanteric fragment (Fig. 1A). Her past medical history was significant for atrial fibrillation (on apixaban). At baseline, she lived at home as a 24-h caregiver and was independent in ambulation with a rollator walker.

Frontal radiographs demonstrating (A) the comminuted left intertrochanteric hip fracture with separate lesser and greater trochanteric fragments (left), and (B) the comminuted left intertrochanteric hip fracture treated with internal fixation with proximally and distally locked short cephalomedullary nails (right).

Duplex ultrasound overlying the left groin demonstrating bidirectional flow in the pseudoaneurysm (i.e. ‘yin-yang’ sign).
Two days after injury, she underwent internal fixation with proximally and distally locked short cephalomedullary nails. The procedure was uncomplicated and completion orthogonal fluoroscopic views confirmed appropriate fracture reduction with hardware in position and intramedullary throughout (Fig. 1B).
On postoperative day 1 (POD), anticoagulation was restarted. On POD6, she was transferred to a rehabilitation institute. Pain was managed with acetaminophen, improved by discharge and the incision healed without complication. On POD27, she completed a course of rehabilitation, was able to walk with a walker and was discharged home with community support.
Unfortunately, due to increasing pain and difficulty weight-bearing, she presented to the emergency room on POD33. She was found to have new left thigh swelling and pain. Deep vein thrombosis (DVT) was ruled out with duplex ultrasound; however, a large left DFA pseudoaneurysm measuring 5.6 cm in length with a neck of 0.4 cm was visualized (Fig. 2). Computed tomography (CT) imaging confirmed a left DFA branch pseudoaneurysm with active extravasation, adjacent to a free-floating osseous fragment, associated with a large thigh hematoma (Fig. 3). In consultation with hematology, her apixaban was not reversed.
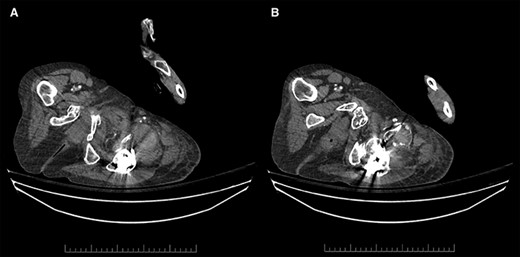
Contrast-enhanced arterial phase axial computed tomographic (CT) images overlying the left hip demonstrating (A) hyperdense material anterior to the left hip in keeping with hematoma (left), and (B) hyperdense material that corresponds to the pseudoaneurysm, which is supplied by a small DFA branch coursing anteriorly and abutting a sharp osseous fragment (right).
Vascular surgery was consulted and CT angiography demonstrated a large DFA pseudoaneurysm (Fig. 4A and B). Given her advanced years and comorbidities, a minimally invasive approach was recommended. The pseudoaneurysm was successfully embolized using numerous microcoils (Fig. 5). Completion angiography demonstrated complete occlusion of the pseudoaneurysm and patent superficial and DFA (Fig. 5). There were no immediate complications. After discussion with the patient, it was agreed that restarting her apixaban increased risk for her hematoma rebleeding and no anticoagulation was continued for stroke prevention.
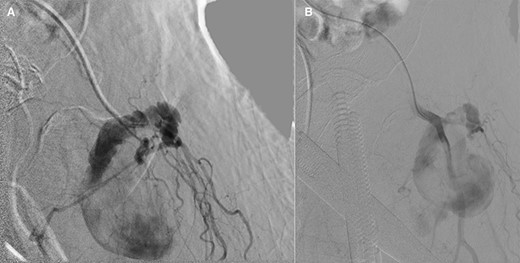
(A and B): Frontal digitally subtracted angiography via a diagnostic catheter positioned in the proximal left DFA demonstrating a large pseudoaneurysm originating from a small DFA branch. The long, narrow and lobulated pseudoaneurysm neck can be see coursing along the cranial aspect of the pseudoaneurysm.

Postcoil embolization digitally subtracted angiography via a diagnostic catheter positioned in the left DFA demonstrating adequate embolization of the injured small DFA branch with complete exclusion of the pseudoaneurysm.
At discharge on POD38, her blood counts were stable and she was pain free and cleared by our allied health team for discharge home.
DISCUSSION
Vascular injury as a complication after hip fracture repair is rare and can be acute or chronic, resulting in massive intraoperative bleeding or formation of a subacute hematoma leading to an arterial pseudoaneurysm [3]. In orthopedics, pseudoaneurysms are caused by direct injury from fractured fragments, dislocation, infection and iatrogenic causes, including surgery [6, 7]. Arterial perforation results in hematoma formation outside the arterial wall, followed by recanalization. Consequently, the pseudoaneurysm sac remains connected to the artery by its ‘neck’ [8]. Risk factors for pseudoaneurysms include age >60 years, female sex, diabetes, hypertension and arteriosclerosis [7].
Time between fracture and clinical manifestation varies and depends on the mechanism of arterial injury, with reports ranging from 3 days to 14 years [5]. Pseudoaneurysms may be caused at time of injury by bone fragments and by over-drilling or improperly positioned retractors during fixation [4]. As the DFA arises posterolaterally from the femoral artery to run down the thigh closer to the femur than the femoral artery, the internal rotation of fracture reduction places the DFA in close proximity to the proximal femur cortex and at increased risk for injury by bony fragments during manipulation. Consequently, ~80% of vascular complications after hip fracture involve the DFA [5]. Delayed injury may be due to chronic erosion of the arterial wall by protruding screws or bony fragment migration [4, 5].
In this case, vascular injury is suspected to be a consequence of proximal migration of the lesser trochanteric fragment. Preoperative imaging demonstrated a separate lesser trochanteric fragment associated with the fracture that was left in situ without fixation at the time of surgery, as is standard practice. Occasionally, there is minor proximal migration of the fragment, but it usually heals in place. It could be hypothesized that migration of the fragment was secondary to the unopposed pull of the iliopsoas cranially as a result of repeated hip flexion. When our patient presented with pseudoaneurysm, CT imaging revealed the fragment had migrated proximally to the level of the femoral head.
Unfortunately, pseudoaneurysms are often not appreciated due to nonspecific presenting symptoms, such as pain and swelling [7]. Due to the deep location of the DFA, clinical signs such as an audible bruit or pulsatile mass are often absent. Diagnosis is further complicated by variability in time between fracture and clinical manifestation and overlapping symptomatology from other complications, such as DVT. Thus, a high index of suspicion is imperative. Diagnosis should be confirmed radiologically through modalities including arterial duplex ultrasound, CT, magnetic resonance imaging or CT angiography.
Management depends on patient comorbidities and pseudoaneurysm location and size. Asymptomatic pseudoaneurysms <3 cm may be monitored in close follow-up for spontaneous resolution [6]. For symptomatic pseudoaneurysms >3 cm, options include open or endovascular repair, embolization or percutaneous thrombin injections. As the majority of patients with hip fractures are elderly and poor surgical candidates, interventional procedures may be preferred to avoid general anesthesia and the morbidity associated with major operations.
In conclusion, this case report highlights the rare but serious complication of DFA pseudoaneurysm after hip fracture fixation. Diagnosis is challenging and often delayed due to nonspecific clinical symptoms. A high index of suspicion is imperative to prevent life-threatening rupture and hemorrhage.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



