-
PDF
- Split View
-
Views
-
Cite
Cite
Sergiy Karachentsev, Blunt vascular trauma in a patient with peripheral arterial disease: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa412, https://doi.org/10.1093/jscr/rjaa412
Close - Share Icon Share
Abstract
Blunt vascular trauma is rare and challenging in management. Trauma victims who are elderly and have medical comorbidities are still uncommon, but their proportion is expected to increase, as life expectancy has been rising worldwide. A case of blunt vascular trauma to the lower extremity in a 70-year-old patient is reported. During the procedure, a contusion of the superficial femoral artery with thrombosis was identified. Besides, the artery was found to be affected by atherosclerosis. Thrombectomy with resection of the artery and end-to-end anastomosis was performed. Good early clinical outcome was achieved. Nonsystematic review of the available literature is also presented.
INTRODUCTION
Every patient with vascular trauma presents a unique situation, which requires an individualized approach and special care [1, 2]. Blunt trauma to the vessels is rare, but notable for its potentially severe consequences including limb loss [3, 4]. Combination of vascular trauma and peripheral arterial disease (PAD) is especially uncommon. The following report presents an unusual case of femoral artery thrombosis caused by blunt injury.
CASE REPORT
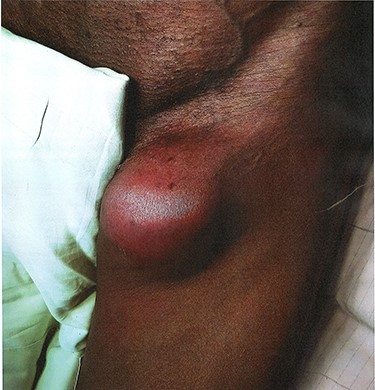
A 70-year-old man came to surgical clinic with complaints of swelling and pain in the left upper thigh developed 8 days ago when he fell down from a bicycle hitting his left groin by the handlebars. He had smoked for 10 years with three to four cigarettes per day, but quit smoking 3 months ago. On examination, a fluctuant nonpulsating mass of about 8 cm in diameter was found in the upper medial left thigh (Fig. 1). Distal pulse was palpable on the contralateral side, brisk in the left groin, but absent in the popliteal region as well as on the foot of the affected extremity. The foot was moderately swollen, painful and numb with decreased skin temperature and limited movement in the toes. Ultrasound revealed ‘a complex cystic lesion in the left groin measuring 7.6 × 6.5 cm; both the femoral vein and artery seen with blood increased in viscosity and slow flow’. The differential included blunt trauma to the left femoral artery with false aneurism alternative haematoma with compression and thrombosis of the femoral vessels. Informed consent for surgical procedure and intraoperative photographs was obtained, and the patient was taken to the operating theatre.
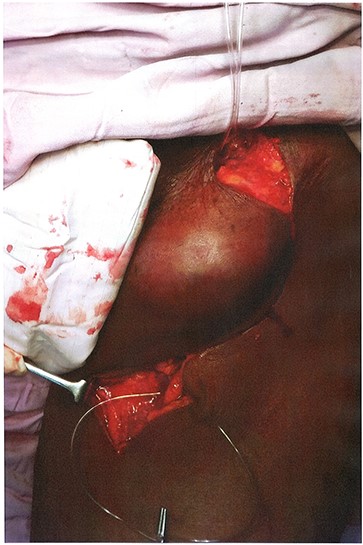
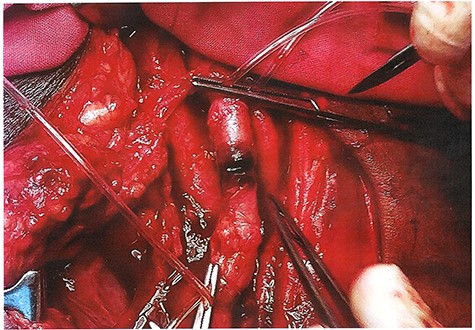
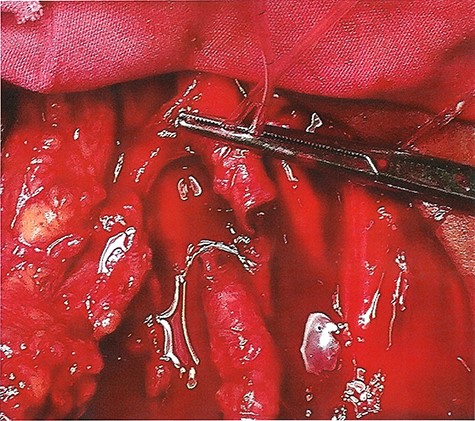
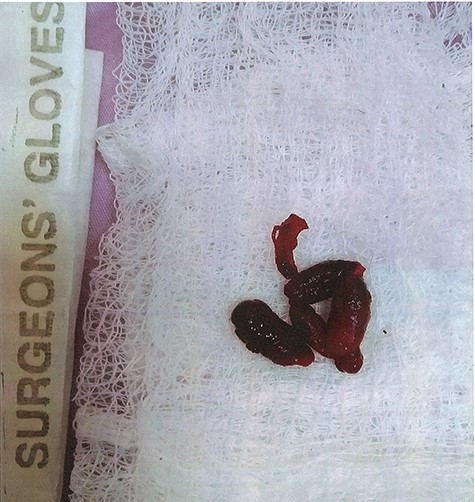
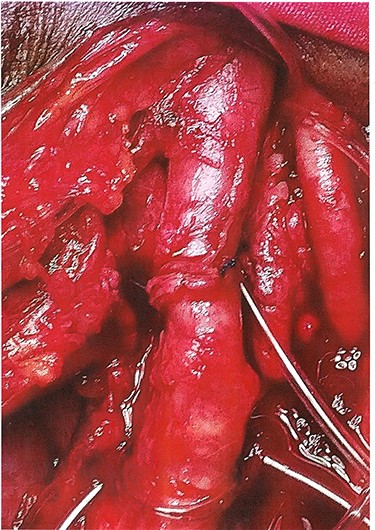
The surgical procedure was performed under spinal anaesthesia. On exploration, after control gained over the common femoral artery above and superficial femoral artery (SFA) below the mass with silastic tubes (Fig. 2), a subcutaneous haematoma of 150 ml of old blood located medially to the trunk of the artery was evacuated. Intramural haematoma with thrombosis of the SFA was found 3 cm distally to the bifurcation (Fig. 3). Femoral vein and deep femoral artery were intact within the wound. SFA was mobilized and transected at the site of injury (Fig. 4), thrombectomy was performed (Fig. 5) with good retrograde flow obtained. A damaged section of 2 cm of the artery was resected. On inspection and palpation, SFA appeared to contain smooth atherosclerotic plaque, albeit without haemodynamically significant stenosis. End-to-end anastomosis with continuous 5-0 polypropylene was performed without tension (Fig. 6) and pulsation of the artery was restored within the wound. Postoperatively, pulse was palpable on the popliteal artery, but distally was absent. Clinical signs of leg ischaemia regressed with swelling disappeared, skin sensation recovered and movements in the toes improved. The patient was discharged home on the 9th day postoperation. He was strongly advised to abstain from smoking and aspirin 100 mg once a day was prescribed. Review in the surgical clinic 31 days postprocedure showed satisfactory pulse on the popliteal artery and signs of good foot perfusion with normal sensation and movements in the toes of the affected leg.
DISCUSSION
Blunt peripheral vascular trauma is rarely encountered by the surgeons and can be particularly challenging in management due to atypical symptoms and often late presentation [5, 6]. Due to improved understanding of injury mechanisms and expanded availability of management options, the outcomes of blunt vascular injury have improved in recent years [3, 5, 7]. Pathophysiologically, blunt trauma-induced arterial injuries frequently result in tunica intima tearing and following obstruction of the lumen by fresh thrombus [8]. Risk of intima disruption and consequent thrombosis increases significantly if the artery is affected by atherosclerosis because of intimal weakening and loss of both elasticity and compliance [9]. In fact, PAD may be present in asymptomatic individuals and can lead to intimal split even in cases of moderate velocity compressive trauma. At the same time, already developed collateral blood supply to the extremity in patients with vascular disease can mitigate acute interruption of axial flow after the main trunk has been damaged. Correspondently, the signs of acute ischaemia in the limb could be minimal or absent even some days after trauma. This is consistent with the findings obtained by Peck and Rasmussen [5] and with the presented case.
Traditionally, the majority of the victims of vascular trauma were young and otherwise healthy [3, 7]. However, it seems that gradual increase of life expectancy in the modern world has inevitably changed the epidemiology of trauma, and victims nowadays appear to be older having a higher incidence of preexisting vascular disease. This trend is corroborated by the recent study of Zhou et al. [6], as four out of eight patients reviewed were >40 years old with the oldest being aged 74. Up to date, literature on blunt vascular injury in patients with PAD is limited to sporadic reports of cases [6, 8].
Presence of arterial occlusive disease in a vascular trauma victim can alter the management plan, opening new possibilities for endovascular treatment. Mini-invasive approach in blunt vascular injury is technically feasible and offers clear benefits in terms of easier access to the target lesion, reduction in blood transfusion requirement and obviation of the potential need for systemic heparinization [6, 10]. Absence of short-term ischaemic necrosis of the affected limb after vascular trauma in patients with atherosclerotic disease is documented in the literature (reviewed in [6]) and confirmed by the current case. This can be attributed to the increased blood inflow to the extremity through the developed system of collateral channels when the axial artery is stenosed or occluded. Thus, the condition gives a time window for appropriate investigation and detailed discussion of the patient in a multidisciplinary team. As some patients would benefit from an endovascular management, transfer to a specialized vascular centre equipped with interventional radiology is to be considered with a low threshold. The counterargument, however, is that every hour of tissue hypoxia increases risk of amputation and death [2, 4], so an optimal balance of time should be sought in every case of blunt vascular trauma.
In conclusion, epidemiology of vascular trauma has been changed in the last decades with victims being older and tending to present with concomitant vascular disease. Individualized approach to the vascular trauma patient with involvement of the multidisciplinary team is to be applied with considerations taken to the mechanism of the injury, anatomy of the lesion and coexistent medical conditions including PAD. Further clinical studies in this area are warranted.
ETHICAL APPROVAL
Permission to conduct the study and to publish the manuscript was sought from the hospital ethical committee.
CONSENT
Written informed consent was obtained from the patient for the procedure and publication of this case report with accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
ACKNOWLEDGMENT
The author acknowledges all the members of the surgical team, information officers and the management of the hospital for their support during the study.



