-
PDF
- Split View
-
Views
-
Cite
Cite
Bharati Pandya, Jason Golmei, Merlyn S Henriques, Anil Dawar, To do or not to do: prolapsed, bleeding, rectal polyp, a dilemma in austere circumstances, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa400, https://doi.org/10.1093/jscr/rjaa400
Close - Share Icon Share
Abstract
Polyps are defined as abnormal growth of tissue from a mucosal surface. Rectal polyps are the most common (2%) cause of gastro-intestinal bleed in children below 10 years. In adults, a rectal polyp presenting as an emergency with irreducible prolapse and massive bleeding causing severe anemia is seldom seen. We present one such case in which surgery was performed under austere circumstances before any investigations, as a life saving measure.
CASE Report
A 40-year-old, female presented to the out-patient with breathlessness and extreme pallor and her mother who accompanied her gave 5 year history of a reducible mass per rectum, which had become irreducible and was bleeding continuously since past 6 days. She was having fainting attacks and was dripping serosanguinous fluid from her anal region. The only investigation she had was a hemoglobin report of 5 g% done 3 days back. She had no significant medical or family history.
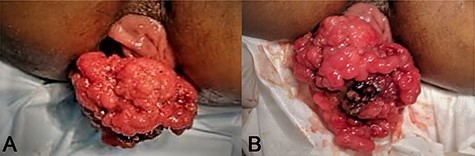
On examination she was grossly pale, had a tachycardia of 110/min, respiratory rate of 24 per min, and systolic blood pressure of 90 mm Hg. Her abdomen was scaphoid with no organomegaly or lump. Rectal inspection revealed a large villous mass (10 x 12 cm size) (Figs 1 and 2) with left anterolateral rectal wall prolapse (Fig. 2B). There was an area of injury (due to finger insinuation) with clot (Figs 1B, 2A and 2C) and the papillomatous polyp was having almost watery bleeding (Fig. 1B) and a thin mucoid discharge.
The patient on presentation had a large prolapsing polypoidal mass per rectum, dragging along with it the anterior wall of rectum. The bleeding was almost watery and there was an area of injury which was due to finger insinuation for reducing the mass. The base of the polyp was wide ~3 x 2 cm from the left antero-lateral wall of the rectum ~6–7cms from the anal verge after resection.
The possibility of getting blood and anesthesia for her immediately was nil, as she was from an extremely poor socio-economic background and had no relatives to arrange for blood, which is the routine pre-requisite for issuing blood in our hospitals. The necessity to stop her bleeding was the top priority, so with explained risks and consent she was given IV analgesia and on a slow drip of lactated ringer, cleaned and draped. The mass was resected with a centimeter margin all around from the visible base of 3 x 2 cm (Fig. 2B) (a third of the rectal circumference) and the rectal wall was sutured with 2-0 interrupted Vicryl. On repositioning of the redundant rectum, the suture line was felt 6–7 cm from the anal verge to the left.
Post-operative course was smooth, and she had no subsequent bleeding or prolapse and on insistence was discharged on the third post-operative day, after arranging and transfusing three units of blood. All her investigations carried out post-operatively were normal, except for an hemoglobin of 3.5 g% which increased to 7.0 g% following transfusions. Her histopathology reported a tubulo-villous adenoma with no evidence of dysplasia. She came back for follow-up after 15 days when her colonoscopy was performed which did not reveal any other polyps. However, she has been kept on regular follow up, and is asymptomatic for 1 year now.
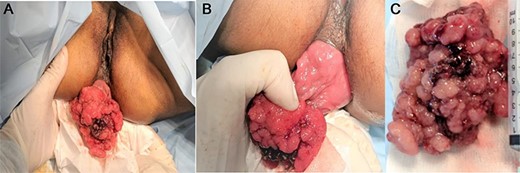
The intra-operative picture of before and after resection of the polyp which was ~10 x 12 cm in size. The finger insinuation injury is seen with clots.
DISCUSSION
In children below 10 years of age, the most common cause (2%) for lower GI bleeds is a rectal polyp [1, 2]. Prolapse of these polyps is also common [1, 2]. The polyps of gastrointestinal tract are defined as macroscopic projection of tissue from a mucosal surface [3].
The importance in understanding colo-rectal polyps lies in their well-established adenoma to carcinoma sequence. Polyps are characterized by their size and morphology (pedunculated or sessile), which are two important features that may predict underlying malignancy and should guide how polyps are managed. The US National Polyp Study defines an advanced adenoma as one that is ≥1 cm in size or contains high grade dysplasia or appreciable villous tissue [3].
Etiologically, polyps may be hamartomatous, inflammatory (or pseudo-polyps), metaplastic or hyperplastic and neoplastic (or malignant), with increasing propensity towards dysplasia in that order [4]. Macroscopically as visualized on endoscopy, polyps could be pedunculated, sessile, flat or depressed with sessile and depressed polyps having a higher incidence of malignancy [4]. Microscopically they could be tubular, tubulo-villous or villous adenomas with increasing incidence of dysplasia and malignancy in that order [3, 4].
Multiplicity is another characteristic of polyps and genetic alterations in forms of proto-oncogene activation, inactivation of tumor suppressor genes and DNA hypomethylation forms the trigger to adenoma–carcinoma sequence [3].
However, <10% of all adenomas turn malignant over a protracted time period of ~8–10 years. But it is equally true, that 95% of colorectal carcinomas develop from adenomas [3]. This forms the basis for investigating, treating and keeping patients under surveillance.
The presentation may range from totally asymptomatic to occult or overt bleeding and symptoms like diarrhea or mechanical obstruction resulting from intussusception or due to the size of the polyp. Hematochezia with mucous discharge or spurious diarrhea could be the presenting feature. Exceptional cases have been recorded where polyps have acted as lead points in rectal prolapse and developed malignancy with prolapse [5] or have even been expelled per rectally [6].
The specific investigations required are stool for occult blood, colonoscopy with biopsy followed by imaging studies in relevant cases. The management of diagnosed patients range from watchful waiting to aggressive surgery. Most of the polyps diagnosed on colonoscopy are either resected endoscopically, keeping the patients on post-resection surveillance, or subjected to surgical resection after biopsy [4]. In cases with massive bleeding, even interventional vascular radiology may be of great help.
Our patient had a unique presentation putting us into a dilemma as to how to manage. We had to resort to absolute austere surgical approach, skipping proper evaluation, even baseline investigations, blood transfusions and anesthesia. Lack of finances and non-availability of blood, ICU facilities and anesthesia in her case were limiting factors. Time was another major factor to be considered, as other than surgical intervention, we had no means to stop the bleeding.
CONCLUSION
Solitary rectal polyps may even present in adults with bleeding and rectal prolapse. The modality of treatment has prescribed protocols in literature. But like in our case, it requires to be catered to the patient specific needs. Our patient underwent an emergency resection of the polyp which turned out to be a benign adenoma; however, the importance of meticulous follow-up in such a large sized polyp cannot be under emphasized.



