-
PDF
- Split View
-
Views
-
Cite
Cite
Tessa Meyer, Patrick Borgen, Kristen Rojas, A spontaneous unveiling of bilateral DCIS in an elderly male, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa399, https://doi.org/10.1093/jscr/rjaa399
Close - Share Icon Share
Abstract
The rarity of male breast cancer continues to limit its study despite increasing incidence rates, particularly within the past decade [Speirs V, Shaaban AM. The rising incidence of male breast cancer. Breast Cancer Res Treat 2009;115:429–30]. Although this trend appears to be substantially documented, male patients with breast cancer have been and continue to be excluded from landmark breast cancer trials. Currently, there are no standardized breast cancer screening protocols in place for men, including those with pathogenic BRCA mutations. As a result, men with breast cancer typically present at a later stage, and on average, 8–10 years later than females [Ruddy KJ, Winer EP. Male breast cancer: risk factors, biology, diagnosis, treatment, and survivorship. Ann Oncol 2013;24:1434–43]. As the incidence of disease continues to rise, the need for algorithmic standardization with regards to screening, diagnosing, treating and managing male breast cancer has become imperative. We report the case of a 71-year-old male who presented with spontaneous bloody nipple discharge and was found to have bilateral ductal carcinoma in situ.
INTRODUCTION
Despite a rising trend in incidence rates over the past 10 years [1], male breast cancer is a rare disease that accounts for ~1% of all cancers in men [2]. Though current research has yet to reveal a definitive cause, present data identifies increasing rates of obesity, alcohol use and ingestion of estrogenic agricultural pesticides as key risk factors [1–3], suggesting that a hyperestrogenic physiologic environment may play a key role in the susceptibility of males to developing breast cancer. Females, however, do ‘not’ appear to be similarly affected. In fact, both the incidence and death rates of female breast cancer have steadily ‘decreased’ over the past two decades, likely attributable to treatment advances, earlier detection and increased awareness [4]. These opposing trends warrant serious reconsideration regarding the current management of male breast cancer.
For decades now, research has suggested the disease process in males to be both biologically and pathophysiologically distinct from those in females [5], yet still the current management of male breast cancer not only negates preventative protocols but also employs treatment methods simply adopted from female-based algorithms. As long as the relative paucity of male data continues to hinder the development of evidence-based, gender-specific alternatives to the current standard of care, the incidence of male breast cancer can only be expected to continue its upward trend.
CASE PRESENTATION
We report the case of a 71-year-old Caucasian male who presented to a nationally accredited comprehensive Breast Health Center with complaints of scant, spontaneous, bilateral bloody nipple discharge over the 4–5 weeks preceding presentation. He denied any associated breast pain, coinciding lesions or masses, use of new medications or supplements, changes in diet, recent illness, unintentional weight loss or recent trauma. Notable past medical history included coronary artery disease and atrial fibrillation (requiring daily use of low-dose aspirin and apixaban, respectively) in addition to hypertension, hyperlipidemia and non-insulin dependent diabetes. Surgical history was non-contributory. Family history was significant for one paternal great aunt and one maternal grandmother with (unspecified) breast cancer.
Initial physical exam was notable for bilateral gynecomastia with expression of scant serous fluid on palpation. Negative findings included any ‘active nipple’ discharge, presence of bleeding, breast tenderness, palpable masses or architectural abnormalities. The patient was referred for further diagnostic workup, beginning with digital mammography. Standard craniocaudal (Fig. 1) and mediolateral oblique (Fig. 2) views of bilateral breasts were performed, which revealed pleomorphic calcifications in the upper outer quadrant of the left breast, as well as amorphous calcifications in the lower inner quadrant of the right breast, consequently affording the patient a Breast Imaging Reporting and Data System score of 4 (suspicious for malignancy) with recommendation for subsequent biopsy.
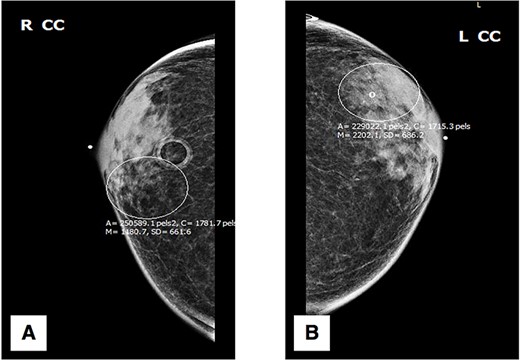
Craniocaudal (CC) mammography: (A) right breast; (B) left breast.
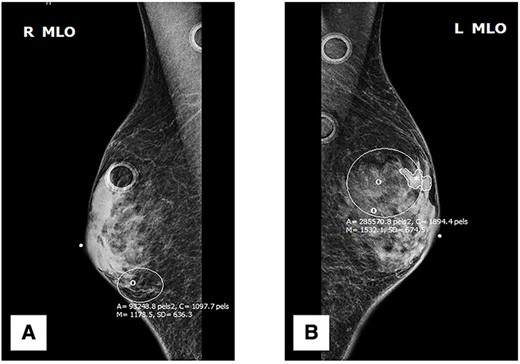
Mediolateral oblique (MLO) mammography: (A) right breast; (B) left breast.
Stereotactic core needle biopsies of both breasts were performed the following week confirming the presence of bilateral intermediate grade ductal carcinoma in situ (DCIS). Subsequent immunohistochemistry staining found both left and right breast cancers to be strongly positive for both estrogen receptor (ER) and progesterone receptor (PR) presence with positive nuclear expression in cell fractions of 90:60% (ER:PR) on the left and 100:100% (ER:PR) on the right. Upon subsequent disclosure of his diagnosis and discussion of recommended treatment options, the patient elected to proceed with a bilateral mastectomy with sentinel lymph node biopsy.
The patient underwent surgery <1 month after initial diagnosis. The surgery proceeded as planned without complications and was well tolerated by the patient. Perioperative management followed the institution-wide opioid-sparing enhanced recovery after (breast) surgery protocol, affording our patient a safe discharge home on postoperative Day 1. Final surgical pathology confirmed bilateral presence of intermediate grade (non-comedo) DCIS with (at least) 3-mm clear margins and negative node involvement (Figs 3, 4), yielding a favorable diagnosis of Tis N0 M0 (Stage 0) disease.
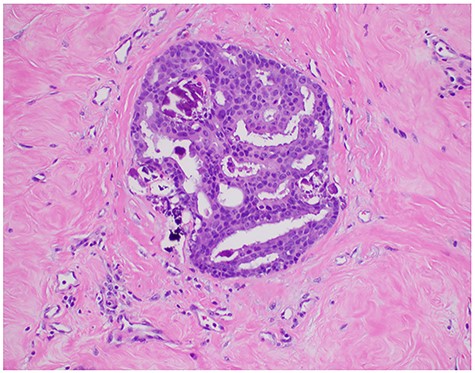
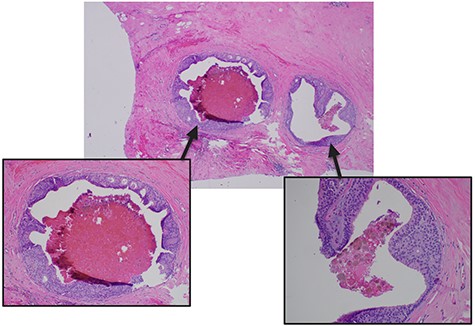
Pathologic microscopy of right breast ductal carcinoma in situ with magnified images highlighting absence of local invasion.
DISCUSSION
The unique disease presentation of our patient places him in a category shared by <10 male subjects throughout the literature [1, 2]. This considered, the medical rarity of our patient rests most heavily on his treatment and prognostic success, in light of the observed outcome tendencies associated with male breast cancer.
Over the past two decades, research has consistently shown distinct biological differences between male and female breast cancers, including a higher frequency of ER, PR and Bcl-2 gene expression, a lower rate of p53 and Erb-B2 gene expression and an increased incidence of BRCA2 gene mutation in males versus females [6, 7]. These differences have been thought to account for variations in pathogenetic evolution and progression of the disease between the sexes [7]. Despite this knowledge, research and data is still considered limited, rendering the current management of male breast cancers subject to the guidance of female-based algorithms, and thus precluding the development of a standardized screening protocol specific to males. As a result, males, on average, are diagnosed with breast cancer 8–10 years later than females and at a later stage, consequently predisposing them to poorer treatment and prognostic outcomes [7, 8].
Despite these documented disparities, tertiary prevention remains the ‘only’ preventative strategy in place as it pertains to male breast cancer. In light of the increasing incidence rates, this course of management is no longer acceptable. Due to unique differences between male and female breast cancer, including but not limited to the pathophysiology, evolution, treatment response and prognostic expectations at various stages along the disease course, it is imperative that we continue to allocate time and resources toward understanding and effectively managing male and female breast cancers as distinct and separate disease entities [9]. In conjunction with more aggressive research initiatives and increased awareness campaigning, it is time we develop a standardized protocol for screening, diagnosing and treating male breast cancer.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



