-
PDF
- Split View
-
Views
-
Cite
Cite
P Bangeas, S Bitzika, P Loufopoulos, K Drevelegkas, V N Papadopoulos, Infarcted ligamentum teres hepatis lipoma mimicking acute abdomen in a female patient: a case report and mini-review of the literature, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa391, https://doi.org/10.1093/jscr/rjaa391
Close - Share Icon Share
Abstract
Lipomas of the ligamentum teres hepatis are extremely uncommon. There have been only a few cases reported in the literature, including lipomas of the falciform ligament of the liver. Here we report a case of torsion and infarction of a lipoma of the ligamentum teres hepatis in a 43-year-old female patient, who presented with acute epigastric pain, nausea and vomiting. Diagnosis was based on computed tomography and magnetic resonance imaging. Patient underwent exploratory laparoscopy followed by laparoscopic excision of the infracted lipoma. Finally, we also provide a mini-review of the literature in order to highlight that although rare, this pathology should be included in the differential diagnosis of acute abdomen.
INTRODUCTION
Ligamentum teres hepatis is embryological remnant of the umbilical vein located in the free edge of the falciform liver ligament [1]. Falciform ligament is a double fold of peritoneum that marks the anatomical division of the two hepatic lobes. Pathological conditions of these two ligaments constitute a rare entity [2–5]. Even though lipomas are very common mesenchymal tumors, only few cases have been reported in the region of ligamentum teres. In this paper, we report a case of a lipoma of the ligamentum teres, that caused acute abdominal pain in a female patient, as a result of torsion and infraction [6–8]. A review of the literature considering this rare entity is also performed.
CASE REPORT
A 43-year-old Caucasian female presented to our emergency department with an acute onset of epigastric pain, nausea and vomiting. Patient temperature and other vital signs were normal. The patient had no relevant medical history apart from three abortions in the last 2 years. Physical examination revealed severe tenderness on the right hypochondriac region and epigastrium while rebound tenderness sign was positive. Her blood test revealed only mild leukocytosis (WBC 11,230 × 103/l).
| Author(s)(Ref.) . | Location . | Year . | Imaging modality . | Management . |
|---|---|---|---|---|
| Adamsen [9] | Ligamentum teres | 1983 | n/a | Surgery |
| Honda et al. [10] | Falciform ligament | 1983 | CT | Surgery |
| Bruneton et al. [11] | Falciform ligament | 1987 | Ultrasound (US), CT | Conservative |
| Budarin [12] | Ligamentum teres | 1988 | n/a | Conservative |
| Farkas et al. [13] | Ligamentum teres | 1991 | n/a | Surgery |
| Kakitsubata et al. [14] | Falciform ligament | 1993 | US, CT, MRI | Surgery |
| Makama et al. [15] | Falciform ligament | 2016 | US | Surgery |
| Author(s)(Ref.) . | Location . | Year . | Imaging modality . | Management . |
|---|---|---|---|---|
| Adamsen [9] | Ligamentum teres | 1983 | n/a | Surgery |
| Honda et al. [10] | Falciform ligament | 1983 | CT | Surgery |
| Bruneton et al. [11] | Falciform ligament | 1987 | Ultrasound (US), CT | Conservative |
| Budarin [12] | Ligamentum teres | 1988 | n/a | Conservative |
| Farkas et al. [13] | Ligamentum teres | 1991 | n/a | Surgery |
| Kakitsubata et al. [14] | Falciform ligament | 1993 | US, CT, MRI | Surgery |
| Makama et al. [15] | Falciform ligament | 2016 | US | Surgery |
| Author(s)(Ref.) . | Location . | Year . | Imaging modality . | Management . |
|---|---|---|---|---|
| Adamsen [9] | Ligamentum teres | 1983 | n/a | Surgery |
| Honda et al. [10] | Falciform ligament | 1983 | CT | Surgery |
| Bruneton et al. [11] | Falciform ligament | 1987 | Ultrasound (US), CT | Conservative |
| Budarin [12] | Ligamentum teres | 1988 | n/a | Conservative |
| Farkas et al. [13] | Ligamentum teres | 1991 | n/a | Surgery |
| Kakitsubata et al. [14] | Falciform ligament | 1993 | US, CT, MRI | Surgery |
| Makama et al. [15] | Falciform ligament | 2016 | US | Surgery |
| Author(s)(Ref.) . | Location . | Year . | Imaging modality . | Management . |
|---|---|---|---|---|
| Adamsen [9] | Ligamentum teres | 1983 | n/a | Surgery |
| Honda et al. [10] | Falciform ligament | 1983 | CT | Surgery |
| Bruneton et al. [11] | Falciform ligament | 1987 | Ultrasound (US), CT | Conservative |
| Budarin [12] | Ligamentum teres | 1988 | n/a | Conservative |
| Farkas et al. [13] | Ligamentum teres | 1991 | n/a | Surgery |
| Kakitsubata et al. [14] | Falciform ligament | 1993 | US, CT, MRI | Surgery |
| Makama et al. [15] | Falciform ligament | 2016 | US | Surgery |
Computed tomography (CT) scan showed a 28 × 13mm solitary mass of fat density, in contact with anterior IV liver segment. Further evaluation with magnetic resonance imaging (MRI) demonstrate an extrahepatic fatty lesion in the anterior perihepatic space adjacent to the falciform ligament (Fig. 1).
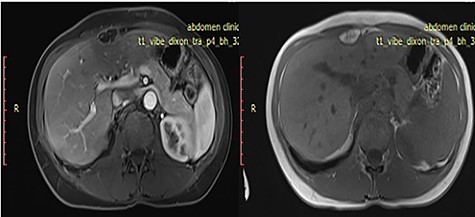
Axial T1 weighted images pre- and post-IV contrast sequences demonstrate extrahepatic fatty lesion in the anterior perihepatic space adjacent to the falciform ligament.
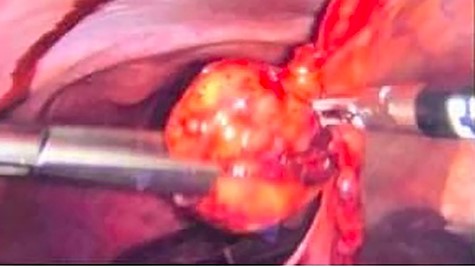
Due to extreme pain of the patient laparoscopic exploration was performed and laparoscopic excision of the twisted lipoma, which was hanging from the ligamentum teres hepatis, followed (Fig. 2). Postoperative period was normal, and the patient was discharged a day after her surgery in very good condition. Final pathological examination reported a CD68 (+) adipose tissue with fibrous septa and inflammatory cells. CD68 is a glycoprotein that is highly expressed in macrophages. Diagnosis of torsion lipoma was histologically confirmed.
DISCUSSION
Falciform ligament is a double fold of peritoneum that contains ligamentum teres, umbilical vein and fat tissue [1]. Pathologies of the falciform and round ligament include internal hernias through congenital or acquired (iatrogenic or traumatic) defects, congenital, infectious, neoplastic or traumatic cysts, inflammatory processes, tumors and tumor-like conditions and intra-abdominal focal fat infarction [2–5]. Although rare, some of these conditions may induce acute abdominal pain, such as isolated abscess, gangrene, necrosis or hematoma of the ligaments and torsion of the fatty appendage [6–8]. Lipomas of the ligamentum teres and the falciform ligament are extremely uncommon therefore only a few cases have been described in the literature. To our knowledge, there have been seven cases reported since 1983 (Table 1), and only in one, there was evidence of infarction causing acute and severe abdominal pain [9].
In majority, patients were asymptomatic, and lipomas were discovered incidentally on imaging during work-up for other pathologies [10–14]. In cases of large lipomas palpate mass could appear during physical examination [10]. Other patients, including our case, presented with signs of the acute abdomen or with a history of chronic epigastric pain [9–15]. In those cases, tenderness was located at the right hypochondriac region and epigastrium. Nausea and vomiting occasionally accompanied the pain. Differential diagnosis, including pancreatic and hepatobiliary diseases, remains a controversial issue. Medical imaging is an essential tool for distinguishing between these conditions.
Sonographic findings include hypoechoic, well-defined lesions with smooth borders at the site of the tenderness, that may displace the stomach [14,15]. Calcifications have also been described [11]. Color flow on Doppler study could also be of help when infarction is speculated. Precontrast CT scan usually discloses a solitary well-marginated mass of fat density with little to no density variation following contrast material injection, thus corresponding to a lipomatous lesion [12–14]. MRI reveals a primary fat signal lesion, heterogenous and hyperintense [14], with characteristics of infarction if present.
Due to severity of the symptoms and/or the size of the mass, surgical excision is usually the treatment of choice [9–15]. Indications pointing toward infarction, as well as call for surgical intervention. Moreover, owing to the rarity of this condition, its non-specific presentation and the fact that sometimes mimics an acute abdomen, not seldom has it been diagnosed intraoperatively during exploratory laparotomy. In our case, exploratory laparoscopy was performed, followed by complete laparoscopic excision of the lesion. Minimally invasive surgery was chosen because of its proven advantages compared with traditional surgery. Pathological examination findings can finally confirm the diagnosis. In all cases, potential malignancy exclusion is mandatory preoperatively.
CONCLUSION
To conclude, lipomas of the ligamentum teres or the falciform ligament of the liver can be an uncommon cause of acute abdomen. Thus, although extremely rare, they should be considered in the differential diagnosis of acute epigastric pain and affirmed by imaging studies, especially by CT and MRI. Preoperative exclusion of malignancy is mandatory. Laparoscopic exploration and excision are the treatment of choice provided it is feasible and safe.
CONFLICT OF INTEREST STATEMENT
None declared.



