-
PDF
- Split View
-
Views
-
Cite
Cite
D A Chávez-Fernández, E Zúñiga-Garza, R A López-Saucedo, Primary tracheal schwannoma resected in a Turner syndrome patient: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa430, https://doi.org/10.1093/jscr/rjaa430
Close - Share Icon Share
Abstract
We report a case of primary tracheal schwannoma in a 31-year-old woman. She had a previous history of follicular thyroid carcinoma treated surgically and Turner syndrome. In a follow-up computed tomography scan, we found a partially obstructing intraluminal tracheal tumor, which was confirmed by bronchoscopy. The patient was treated by surgical resection and primary tracheal anastomosis. The tumor was 14 mm in diameter, with an intact capsule. Histologic analysis revealed a Schwann cell origin tumor.
INTRODUCTION
Primary tracheal tumors are uncommon and most of them are malignant. Altogether, squamous cell and adenoid cystic carcinoma represent >75% of the cases [1]. Neurogenic tumors arising from the peripheral nerves represent one of the varied origins of benign tumors. These are divided into schwannoma and neurofibroma. Schwannomas in the trachea are extremely rare, being more frequent in lung parenchyma or bronchi [2]. In most cases, diagnosis may be delayed because of the insidious and non-specific symptoms [3]. We present a clinical case report from a patient with a primary tracheal schwannoma treated by surgical resection.
CASE REPORT
A non-smoker 31-year-old female with a history of Turner syndrome and Follicular thyroid carcinoma treated by total thyroidectomy and radical neck dissection, presented to her follow-up visit at the oncology department. The patient did not report symptoms such as dyspnea, cough, wheezing, or neck masses. No tumors or abnormal breath sounds were present during the physical examination. The follow-up computed tomography (CT) scan incidentally showed a partial airway obstruction secondary to a 14 mm endotracheal tumor (Fig. 1). There were no lymphadenopathy or mediastinal masses. Flexible bronchoscopy confirmed a 14 × 8 × 5 mm, smooth and oval-shaped tumor at the left posterior tracheal wall.
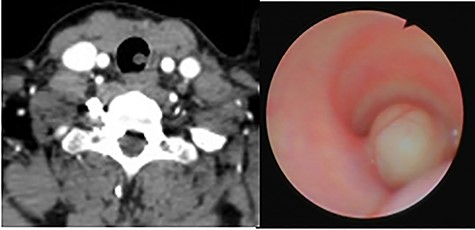
(A) CT scan showing an endotracheal tumor at the left posterior tracheal wall; (B) bronchoscopy view showing partial airway obstruction caused by the tumor.
The patient was submitted for surgical resection by an anterior cervical approach. During surgery, the identification of the tumor was made by bronchoscopy. The anterior tracheal wall was incised distally to the tumor at the level of the fourth tracheal ring and the tumor was resected at its pedicle (Fig. 2). The tracheal wall was closed with interrupted 3–0 polydioxanone stitches. A closed, active Blake drain was left in the paratracheal space to avoid subcutaneous emphysema. It was removed on the seventh postoperative day.

(A) Anterior tracheotomy at the fourth tracheal ring; (B) gross resection specimen.
The histologic examination showed an Antoni A cellular pattern, composed of spindle cells with palisading nuclei areas, without mitotic activity or necrosis areas, being compatible with schwannoma (Fig. 3).
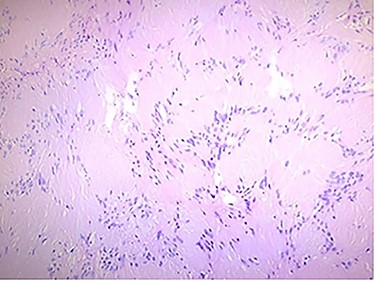
Histologic findings: the tumor was formed by spindle cells with elongated palisading nuclei; hematoxylin and eosin stain.
Four weeks later, a control bronchoscopy showed a normal healing process, without stenosis or tumor persistence at the surgical site (Fig. 4). Two months after surgery, the patient resumed her daily life activities. At present, 14 months since the procedure, the patient continues asymptomatic, with a normal functional status, and still under clinical surveillance without local recurrence.

Bronchoscopy view at the tumoral resection site after 4 weeks from surgery.
DISCUSSION
Primary tracheal tumors are less frequent than bronchial tumors. Within the several histologic types, neurogenic origin tumors are extremely rare. Since the first tracheal schwannoma report by Straus in 1951 [4], only a few cases have been described. In 2015, a systematic review found 51 reported cases with tracheal schwannoma [5]. Between 2015 and 2020, only five cases have been reported in English literature [6–10].
Symptoms may vary according to size, location and degree of airway obstruction [2, 3, 5]. In most cases, clinical manifestations are insidious and non-specific, making diagnosis difficult [4]. Commonly reported symptoms are dyspnea, cough and wheezing [3, 5], while some patients may initially remain asymptomatic, like the present case.
CT scan and bronchoscopy are usually made to confirm the diagnosis and to evaluate the tumor extension. Other useful diagnostic methods are pulmonary function test and positron emission tomography scan [8].
The prognosis for patients after primary resection is usually favorable [5] and currently it is the treatment of choice, either by open or endoscopic approach. The former is usually preferred if there is an extratracheal extension or a recurrent lesion, while the latter is better for pedunculated tumors, with no extratracheal extension and high surgical risk patients [3,7]. The possibility of recurrence after endoscopic excision must be considered.
To the best of our knowledge, this is the first primary tracheal schwannoma resected and reported case in Mexico.



